Indice del volumen
Volume index
Comité Editorial
Editorial Board
Comité Científico
Scientific Committee
NEURO-BEHCET'S SYNDROME TREATED WITH HERBAL MEDICATION.
*Foyaca-Sibat H, **Ibañez-Valdés LdeF.
*Department of Neurology, **Department of Family Medicine.
University of Transkei. Umtata. South Africa.
foyaca @ intekom.co.za
Rev Electron Biomed / Electron J Biomed 2003;1(3):161-169.
- Saenz A, Ausejo M, Shea B, Wells G, Welch V, Tugwell P. Pharmacotherapy for Behcet's syndrome (Cochrane Review): http://www.update-software.com/abstracts/ab001084.htm)
- Saenz A, Ausejo M, Shea B, Wells G, Welch V, Tugwell P. Abstract of review Vasculitis: Pharmacological Therapy for Behcet's Syndrome. http://www.nihs.go.jp/dig/cochrane/jp_9802/revabstr/ab001084.htm
Comment Reviewer Dr. Felix Conde Martín. Hospital Can Misses. Ibiza. España
Comment Reviewer Prof. Fidel Fernández Fernández. Universidad de Cantabria. Santander. España.
Abstract
We report a case fulfilling the diagnostic criteria of Behçet’s disease (BD) with a intracerebral hemorrhage who improve from this cerebrovascular complication and remained free of BD activity for more than two years after be treated traditionally. The authors believe it is an anecdotic report but herbal medicines probable can be useful in the management of patient with this condition.
KEY WORDS: Neuro-Behçet, intracerebral hemorrhage, herbal medication.
Introduction.
A Turkish dermatologist Hulussi Behçet described this pathological process in 1937. Most of the confirmed patients have been identify along the ancient Silk Road which extend from Eastern Asia and Middle East to the Mediterranean basin1 and most of the papers presented on the 10th International Congress on Behçet's Disease held in Berlin during June 27-29, 2002 based on epidemiology, reported a higher prevalence of Behçet’s disease (BD) in the above-mentioned countries2. Epidemiological findings suggest that both genetic and environmental factors influence the pathogenesis of the disease. BD is a rare and chronic condition of unknown cause that affects in young peoples the inner lining of the mouth and genitals and the small blood vessels all over the body including eyes and brain among others, causing recurring mouth and genital ulcers; those sores can occur in the tongue, and on the inside of the lips and cheeks usually lasting for one to three weeks, the genital ulcers appear less often than the mouth sores and they are sometimes mistaken for herpetic lesions; skin involvement is also common. Uveitis and retinitis causing blindness can be present, also arthritis, peripheral vasculitis and neurological complications often called Neuro-Behçet’s Syndrome (NBS). Clinical criteria for the diagnosis of BD3 are summarized in Table I.
Pallis and Fudge4 in 1956 and Wadia and Williams5 in 1957, described the clinical manifestations of NBS for the first time and they established three different types such as: 1) Brainstem disturbances, 2) Meningomyelitis, and 3) Confusional syndrome, dementia, Parkinsonism, pseudobulbar palsy and quadriparesis. Vascular complications as a result of vasculitis of the vasa vasorum or dural venous sinus thrombosis, intracranial hypertension, polymiositis, and peripheral neuropathy, spinal cord lesions, optic neuropathy6, and vestibulocochlear involvement have been reported7.
In 5 to 50 percent of patient with BD a chronic and progressive involvement of the nervous system mainly in male patients in whom the disease began at an early age, are present. Neurological involvement is either caused by primary neural parenchyma lesion (Neuro-Behçet) or secondary to major vascular involvement (Vasculo-Behçet).
The course is relapsing-remitting, secondary progressive or primary progressive and the most commonly affected area is the brain stem with other additional symptoms or signs, and hemispherical involvement with mental changes. Factors suggesting a poor prognosis are repeated attacks, incomplete recovery, progressive disease course, and high level of CSF leucocytosis during acute attack8. Erectile dysfunction secondary to NBS is well known, and without neurological involvement has been reported recently.9 Cerebrovascular complications in BD are unusual, however some patients with ischemic stroke, cerebral vaculitis, subarachnoid hemorrhage and intracerebral hemorrhage have been documented, and published.10-18 In 2002, Kikuchi18 reported three cases of NBS presenting with intracerebral hemorrhaging and divided them into two groups: cerebrovascular or cyclosporine related.
More than 55 percent of patients with NBS are positive for HLA-B51 allele, levels of circulating tumor necrosis factor alpha, interleukin-1 beta, and interleukin-8 have been reported to be elevated and their lymphocyte function is abnormal.19
The aim of this article is to report a case with clinical and radiological manifestation of NBS and his outcome after being treated traditionally.
Report of a case.
A 29 years-old male patient was born as a second child to healthy non-consanguineous parents parents from The Kingdom of Khosa and The Kingdom of Zulu. Pregnancy and birth were normal. His relatives referred a previous history of successfully treated pulmonary tuberculosis while he was working in a gold mine two years ago. They also said that he was on anti- epileptic treatment for recurrent right focal simple motor seizures of unknown cause and he was also taking "pills" for recurrent ulcers on his mouth and genital region.
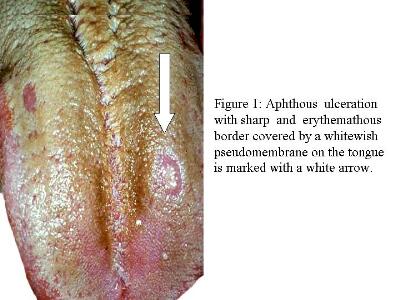
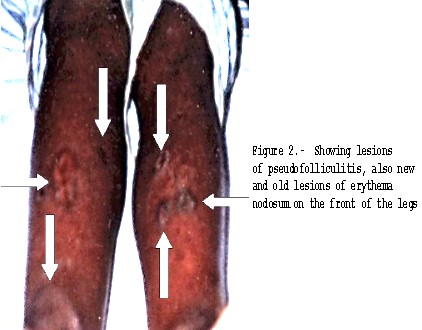
On the admission day the patient was brought by her parents to Umata General Hospital (tertiary neurological care services for 6, 4 million of peoples) and admitted in its male Stroke Unit in comatose stage. The family history was unremarkable. On examination some aphthous ulcerations on the tongue and gingival region are seen (Figure 1) also reddish bumps, pimples sores on both legs were present (Figure 2) some acneiform nodules all over the back, neck and face were also seen.
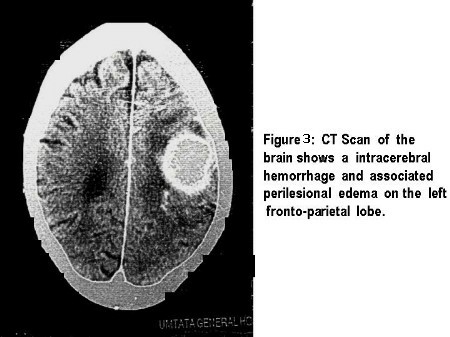
His head circumference was 57 cms, he was deeply unconscious his pupils isochoric and more reactive to light stimulation on the right side compare with the left, no deformation of the iris or signs of retinopathy were not found. Babinski sign and other motor signs on the right hemi body, ipsilateral central facial palsy, doll’s eyes response and ciliospinal reflexes were present. Horizontal nystagmus was absent on caloric test. No signs of decerebrate or decorticate positioning were detected, and no other cranial nerves were involved. Cardio respiratory system was intact. CT Scan of the head showed an intraparechymal hemorrhage on the left put amen region and associated processional edema (Figure 3).
Other laboratory test doesn’t show abnormalities. A diagnosis of vasculo-NBS was made. After the medical, physical and supportive treatment the patient began to improve gradually and was discharged home seven weeks later walking with support. Unfortunately the skin lesions and recurrent ulcers did not improve remarkably in spite of treatment.
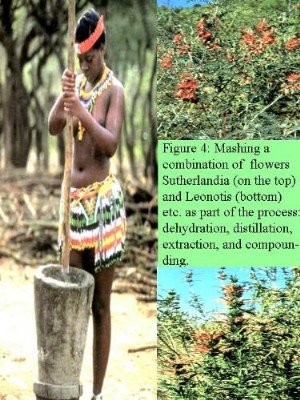
At this point the patient went to traditional healer (Sangoma) for treatment and after five months therapy with Vulindaba: a combination of two powerful plants: Sutherlandia and Leonotis (Figure 4), formulated by Sanusi Vusamazulu Credo Mutwa. After that course of herbal medicines apart from some irritation of the skin after shaving, no more signs of Behçet’s activity for the past two years were observed.
COMMENTS.
Inrtacerebral hemorrhage is extremely rare vascular complication of NBS and this report should be considered as an anecdotic coincidence. BD is a very rare disease in Sub-Saharan Africa countries compare with its incidence and prevalence in patients of North Africa origin.20
Apart from genetic factors other than HLA-B51 a linkage on chromosome 16 and 12 seems to be present in multicase families with BD along the ancient Silk Road countries; other findings related with -403 AA haplotype of the chemokine RANTES, -2516 AA, -2076 AA halotypes of the MCP-1 chemokine, TNF-1031 allele, ICAMI 489*E variant, methylation of genes, TTbb phenotype, and MEVF mutations in patients with BD serve to support the immunogenetic mechanism in the pathogenic of BD. There was a general consensus among the immunological studies presented in the above-mentioned congress that the inflammatory reaction in BD has mainly a Th1 cytokine profile,2 therefore environmental conditions, nutritional aspects, and associated infections can play an important role in the pathogenesis of this process and its geographical distribution.
Current tendencies for treatment of BD are focusing on interferon and tumor necrosis factor-alpha, although pentoxifylline, cyclosporine, and azathioprine remain its validity.
In South Africa more than 75% of the population use traditional medicine on regular basis, those herbal medicines can be gathered in many regions and combined at home, can be bought from herbal sellers in urban areas,21 or even can be ordered by phone21 This Muti was created and used successfully by Sanusi Mutwa family for over hundred years for the treatment of all sorts of ailments such as: Depression, Stress, Cancer, Tuberculosis, Rheumatoid arthritis, Headache, etc. It is a appetite stimulant enhances well-being, it is also mild aphrodisiac, and also builds up the immune system; it is not only non toxic and with no adverse side effects it is also affordable to the peoples that need it most and have not other choice because of their extreme poverty.22 There is a general concern about the role played by Vulindaba in immunocompromised patients, and new alternative ways to fight HIV/AIDS are under discussion between sangomas’ populations. (Figure 5).
The Behçet’s Current Activity Index has been described elsewhere23 and is a useful way for measurements the BD’s outcomes; in our patient absent of BD activity for more than two years is "a successful respond" to herbal medication. The marked geographical differences in disease expression of BD, as well as possible ethnic and intercultural differences in disease impact among individuals from different geographical regions, require the evaluation of this results in other countries before recommending its therapeutic use universally, also a randomized, double-blind placebo trial’s results should be considered.
REFERENCES.
1. - Kaklamani VG, Variopoulos G, Kaklamani PG. Behçet's disease. Semin Arthritis Rheum 1998;27:197-217.
2.- Fresko I. Highlights of the 10th International Congress on Behçet's Disease.Clin Exp Rheumatol 2002;20(4):200-216.
3.- International Study Group for Behçet’s disease. Lancet 1990;335:1078-1080.
4.- Pallis CA, Fudge BJ. The neurological complications of Behçet’s syndrome. Arch Neurol.Psychiatric 1956;75:1-14.
5.- Wadia N, Williams E. Behçet’s syndrome with neurological complications. Brain 1957;80:59-71.
6. - NakamuraT, Takahashi K, Kishi S. Optic Nerve Involvement in Neuro-Behçet’s Disease. Jan J Ophthalm 2002; 46(1):100-102.
7. -Kidd D, Steuer A, Denman AM, Rudge P. Neurological complications in Behcet’s syndrome. Brain 1999;122(11):2183-2194.
8. - Serdarogu P. Behçet’s disease and the nervous and the nervous system. J. Neurol 1998;245(4):197-205.
9. - Aksu K, Keser G, Gunaydin G, Ozbek SS, Colakoglu Z, Gumusdis G, Dogavaasargil E. Erectile dysfunction in Behçet’s disease without neurological involvement: two case reports. Rheumatology 2000;39:1429-1431.
10. -Iragui VJ, Maravi E. Behçet’s syndrome presenting as cerebrovascular disease. J Neurol Neurosurg Psych 1986; 48:838-840.
11. - Buge A, Vincent G, Rancurel D, Dorra M, Beourne C. Maladie de Behçet avec anevrysmes arteriels multiple intracraniens. Revue Neurologique 1987;143:832-835.
12.- Zelenski JD, Capraro JA, Holden D, Calabese LH. Central nervous system vasculitis in Behçet’s syndrome: angiographic improvement after therapy with cytotoxic agents. Arth Rheumat 1989;32:217-220.
13. - Matsumoto T, Uekusa T, Fukuda Y. Vasculo-Behçet’s disease: a pathologic study of eight cases. Human Pathol 1991;22:45-51.
14. - Nishimura M, Satoh K, Suga M, Oda M. Cerebral angio-and neuro-Behçet’s syndrome: neuroradiological and pathological study of one case. J Neurol Sci 1991;106:19-24.
15. - Bahar S, Coban O, Guvit IH, Akman-Demir G, Gokyigit A. Spontaneous dissection of the extracranial vertebral artery with spinal subarachnoid hemorrhage in a patient with Behçet’s disease. Neuroradiology 1993;35:352-254.
16. - Akman-Demir G, Serdaroglu P, Tasçi and the Neuro-Behçet Study Group. Clinical patterns of neurological involvement in Behçet’s disease: evaluation of 200 patients. Brain 1999;122:2171-2181.
17.- Krespi G, Akman-Demir G, Poyraz M, Tugcu B, Coban O, Tucay R, Serdaroglu P, Bahar S. Cerebral vasculitis and ischemic stroke in Behçet’s disease: report of one case and review of the literature. Eur J Neurol 2001;8(6):719-723.
18. - Kikuchi S, Niino M, Shinpo K, Terae S, Tashiro K. Intracranial hemorrhage in neuro-Behçet’s syndrome. Intern Med 2002 Sep;41(9):692-695.
19. - Sakane T, Takeno M, Suzuki N, Inaba GI. Behcet’s Disease. The New Eng. J. Med 1999;341(17):1284-1291.
20. - Krause I, Mader R, Sulkes J, Paul M, Uziel Y, Adawi M, Weinberger A. Behçet’s disease in Israel: the influence of ethnic origin on disease expression and severity. J Rheumatol 2001May;28(5):1033-1036.
21.-Foyaca-Sibat H, Ibañez-Valdés LdeF. Acute renal failure due to herbal medicine intoxication in acquired neuromyotonia. 2nd International Congress of Nephrology in Internet. Available on: http://www.uninet.edu/cin2001/paper/ibanez/foyaca.html.
22.-Mutwa SVC. Sangomas unite to fight Aids traditionally. IZWILETHU 2002;1(30):21.
23. - Bhakta BB, Brennan P, James TE, Chamberlain MA, Noble BA, Silman AJ. Behçet’s disease: evaluation of a new instrument to measure clinical activity. Rheumatology 1999;38:728-733.
Comment Reviewer Dr. Antonio Felix Conde Martín. Hospital Can Misses. Ibiza. España aconde @ hcm-ibiza.es
Classical Behçet´s disease is a multisystemic, chronic, recurrent inflammatory disorder characterized as a triad of hypopyon uveitis, oral aphthae and genital ulcers. Clinical criteria for the diagnosis of Behçet´s disease are well established as the authors remark.
The patient presented, was admitted because of an extremely rare event (cerebral haemorrhage) in this disorder. In my opinion, such a case should fit better to clinical criteria than any other to be really convincing. Neuron-Behçet´s disease typically manifests late after disease onset and often heralds a poor prognosis for survival. There is an obscure history of seizures and anti-epileptic treatment which is not detailed at all. The authors also do not detail nothing about which treatment was administrated after the diagnosis of Behçet´s disease was made.
The pictures presented are, with exception of the one of the tongue, of poor quality.
Comment Reviewer Prof. Fidel Fernández Fernández. Universidad de Cantabria. Santander. España. apafff @ humv.es
Los autores describen un caso de enfermedad de Behçet con afectación cerebral (tipo Vásculo-Behçet) que remite tras terapia con Vulindaba.
La enfermedad de Behçet es una enfermedad de evolución crónica e intermitente, con fases de remisión y recidiva que pueden durar entre semanas y años e incluso se puede prolongar durante décadas.
A veces se presentan complicaciones neurológicas (denominadas Neuro-Behçet o Vásculo-Behçet):
http://www.acnr.co.uk/pdfs/volume3issue1/v3i1reviewart1.pdf
http://www.rad.upenn.edu/~herskovi/Course1999/manifsystdis/Behcet.html
http://www.greenprac.ndtilda.co.uk/jamie/Behcets%20Syndrome.html
http://www.scielo.br/pdf/anp/v59n2A/a20v592a.pdf
Una magnífica revisión de la enfermedad aparece en http://www.usagiedu.com/articles/html/beh/beh.pdf
También se puede obtener información detallada en http://www.nlm.nih.gov/medlineplus/behcetssyndrome.html
El tratamiento es sintomático y empírico. Muchos de los fármacos utilizados (http://www.behcets.com/treatments.ivnu ) son de eficacia cuestionable:
de ahí que, en países donde tienen una amplia tradición en tratamientos alternativos, hayan valorado la utilidad de plantas autóctonas, entre ellas Sutherlandia Frutescens y Leonotis leonurus. La Sutherlandia Frutescens posee importantes principios activos (L-canavanina, pinitol y ácido gama-amino-butírico), algunos de los cuales, al inhibir la sintetasa de oxido nítrico, podrían explicar sus beneficios en casos de inflamación crónica:
http://www.adaptogeno.com/bol_svms1.htm#Item5
La descripción de un solo caso, con interesantes ilustraciones, de la regresión de la enfermedad no permite extraer conclusiones sobre la eficacia o no de la terapia con Vulindaba, como los mismos autores señalan, siendo necesario ensayos clínicos randomizados.
