Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
- Fractional excretion of Potassium (K): FEK = [K urine x serum creatinine / serum K x urinary creatinine] x 100
- Trastubular Potassium Gradient (K): TTKG = [urinary osmolality x serum creatinine / serum osmolality x urinary creatinine]
ASSESSMENT OF THE TUBULAR HANDLING OF POTASSIUM IN CIRRHOTIC PATIENTS TREATED WITH A COMBINATION OF FUROSEMIDE + SPIRONOLACTONE
Musso C1, Casciato P2, Gaite L2, Vilas1, Navarro M1, Martinez B3, Rivera H1, Luxardo R1, Algranati L1, Gadano A2
1Nephrology Service and 2Hepatology Department of the 3Internal Medicine Service.
Hospital Italiano de Buenos Aires. Argentina
carlos.musso @ hospitalitaliano.org.ar
Rev Electron Biomed / Electron J Biomed 2011;3:39-43.
Comment of the reviewer Dr. Abdias Hurtado Arestegui . Department of Nephrology. Hospital Nacional Arzobispo Loayza. Universidad Peruana Cayetano Heredia. Lima. Peru
Comment of the reviewer Dra. Rossina Elizabeth Juarez. Specialist in Medical Clinics, Nephrology. Peritoneal Dialisis and Renal Phisiology.
SUMMARY:
Cirrhotic patients develop hyperaldosteronism secondary to advanced stages of their illness and require treatment with furosemide + spironolactone. The tubular handling of potassium (K) in this patients under such combined diuretic scheme (antagonic) had not yet been studied, therefore we decided to document in an original way the net effect, in this pharmacological context, of the renal potassium handling assessed by means of two specific indicators for that purpose: the fractional excretion of potassium (FEK) and the trastubular potassium gradient (TTKG).
Material and Method: The FE of sodium (Na), FEK and TTKG were assessed in 18 patients (11 men), with an average age of 56, normokalemic, suffering from compensated cirrhosis (Ci) stages Child Pugh A, B and C, MELD 22, having normal glomerular filtration, urinary sediment and renal ultrasound, treated with furosemide (average dose: 40 mg/day) + spironolactone (average dose: 100 mg/day) and on hyposodic diet. The control group consisted of 10 healthy volunteers under the same diet (S). For the statistical analysis of the data, the non-parametric test Wilcoxon was applied.
Results: Kalemia (mmol/l): 4 ± 0.5 (Ci) vs. 4 ± 0.3 (S), p=NS; FENa (%): 0.8 ± 0.4 (Ci) vs. 0.5 ± 0.3 (S) p=NS; FEK (%): 9.1 ± 3 (Ci) vs. 10 ± 2 (S), p=NS; TTKG: 6 ± 2 (Ci) vs. 4 ± 1 (S), p=0.04.
Conclusion: It was documented a significant urinary potassium excretion increase in cirrhotic patients on furosemide + spironolactone, only detected by the TTKG.
KEYWORDS: Potassium. Cirrhosis. Transtubular potassium gradient
RESUMEN:
Los cirróticos desarrollan hiperaldosteronismo secundario en estadios avanzados de su enfermedad, requiriendo tratamiento con furosemida + espironolactona. El manejo tubular del potasio (K) en estos pacientes bajo dicho esquema diurético combinado (antagónico) no ha sido aun estudiado, por lo cual decidimos describir el valor de la excreción fraccional (EF) de potasio y del gradiente transtubular de potasio (GTTK) en esta población bajo dichos diuréticos.
Material y Método: Se evaluó prospectivamente la EF de sodio (Na), EFK y GTTK en 18 pacientes (11 hombres), edad promedio 56 años, normokalémicos, cirróticos (Ci) compensados estadios Child Pugh A, B y C, MELD medio 22, portadores de filtrado glomerular, sedimento urinario y ecografía renal normales, tratados con furosemida + espironolactona y dieta hiposódica. Grupo control: 10 voluntarios sanos bajo igual dieta (S). Análisis estadístico: Wilcoxon.
Resultados: Kalemia (mmol/l): 4 ± 0.5 (Ci) vs. 4 ± 0.3 (S), p=NS; EFNa (%): 0.8 ± 0.4 (Ci) vs. 0.5 ± 0.3 (S) p=NS; EFK (%): 9.1 ±3 (Ci) vs. 10±2 (S), p=NS; GGTK: 6 ±2 (Ci) vs. 4 ±1 (S), p=0.04.
Conclusión: Observamos que en cirróticos tratados con furosemida + espironolactona, existe un incremento significativo de la excreción urinaria de potasio, sólo evidenciable por el GTTK.
PALABRAS CLAVE: Potasio. Cirrosis. Gradiente transtubular de potasio.
INTRODUCTION:
Cirrhotic patients develop hyperaldosteronism secondary to advanced stages of their illness and require treatment with furosemide + spironolactone.
The tubular handling of potassium (K) in this patients under such combined diuretic scheme (antagonic) had not yet been studied, therefore we decided to document in an original way the net effect, in this pharmacological context, of the renal potassium handling assessed by means of two specific indicators for that purpose: the fractional excretion of potassium (FEK) and the trastubular potassium gradient (TTKG)1-4.
MATERIAL AND METHOD:
The FE of sodium (Na), FEK and TTKG were assessed in 18 patients (11 men), with an average age of 56, normokalemic, suffering from compensated cirrhosis (Ci) stages Child Pugh A, B and C, MELD 22, having normal glomerular filtration, urinary sediment and renal ultrasound, treated with furosemide (average dose: 40 mg/day) + spironolactone (average dose: 100 mg/day) and on hyposodic diet. The control group consisted of 10 healthy volunteers under the same diet (S). For the statistical analysis of the data, the non-parametric test Wilcoxon was applied.
The formulae used were:
RESULTS:
Regarding serum potassium value, no significant difference was documented between the studied groups:
- Kalemia (mmol/l): 4 ± 0.5 (Chirrhotic) vs 4±0.3 (Healthy), p=NS
There was no significant difference neither in the FENa nor in the FEK, between the studied groups:
- FENa (%): 0.8 ± 0.4 (Chirrhotic) vs. 0.5± 0.3 (Healthy) p=NS;
FEK (%): 9.1 ±3 (Chirrhotic) vs 10±2 (Healthy), p=NS
Nevertheless, a significant difference was identified in the TTGK between these groups, having a significant higher value in the cirrhotic one:
- TTKG: 6 ±2 (Cirrhotic) vs 4±1 (Healthy), p=0.04.
DISCUSSION
Thick ascending loop of Henle is a segment which is impermeable to water and urea, but permeable to sodium since it has an apical transporter NaK2Cl (which, as indicates its name, cotransports potassium and chloride along with sodium), and whose gradient is given by the existence of a NaKATPase baso-lateral pump. This determines that in this sector a 40% of the sodium filtrated at a glomerular level will be reabsorbed, and that hypotonic urine will be produced, so this is considered to be the sector of the nephron where free water clearance is generated. Therefore, the osmolarity in urine at the end of this segment is around 100 mOsm/l. On the other hand, the same mechanism which contributes to generate the concentration of sodium at a medullar level, and thus, is the driving force of the so called countercurrent mechanism which generates medullar hypertonicity (Figure 1).
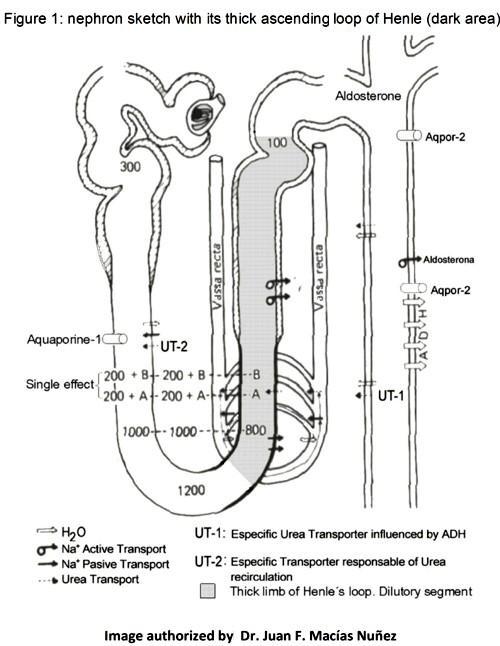
Then, when furosemide blocks the NaK2Cl cotransporter, it induces an increase in sodium excretion, which leads to a state of contraction of volume with the subsequent secondary hyperaldosteronism, which is ultimately the one which ends up producing an increase in the renal excretion of potassium4.
The collecting tubule is a segment where approximately a 3-5% of the sodium filtrated is reabsorbed, by means of sodium channels located in the apical pole of the tubular cells; thanks to a concentration gradient generated by a NaKATPase baso-lateral pump. Sodium (cation) reabsorption through the apical cell makes the luminal tubular surface relatively negative in comparison to the intracellular one. Simultaneously, the intracellular potassium is secreted towards the light, through a potassium channel, following an electric and chemical gradient: the electric gradient is based on the luminal electronegativity and the chemical one is based on the high intracellular potassium concentration due to the action of the basolateral pump. All this above mentioned mechanism is intensified in presence of serum aldosterone, which stimulates the increase in number and the function of the sodium and potassium channels as well as the NaKATPase pump of the principal cells, inducing not only higher sodium reabsorption but also a higher secretion of potassium. Spironolactone, an inhibitor which competes with the aldosterone for its receptor, leads to the opposite effect: the loss of sodium and saving of potassium5.
The cirrhotic patient in an advanced state usually receives both of the aforementioned drugs (furosemide + spironolactone), which have an antagonic effect regarding the tubular handling of potassium 5-6.
This study documented that in cirrhotic patients on a pharmacological context of furosemide (40 mg/day) + spironolactone (100 mg/day), there was a net increase in the urinary potassium excretion6-8
The fact that the TTKG was more sensitive to detect the increase in potassium excretion in this population could be precisely explained by the fact that TTKG is a better index than the FEK, since this index corrects the phenomenon of the distal handling of potassium related to the one being carried out with water at such level. The water excreted by means of the furosemide dilutes the urinary potassium and underestimates its magnitude of urinary secretion, which the FEK cannot control while TTKG can2.
CONCLUSSION: It was observed that in cirrhotic patients treated with furosemide + spironolactone, there was a significant urinary potassium excretion, which was only made evident by means of the transtubular potassium gradient.
REFERENCES
-
1.- Adrogue H, Wesson D. Potassium. Houston. Libra & Gemini. 1992
2.- Halperin M, Goldstein M. Fluid, electrolyte, and acid-base physiology. Philadelphia. Saunders. 1999
3.- Clarkson M, Magee C, Brenner B. Brenner & Rector. The Kidney. Philadelphia. Saunders. 2010
4.- Rennke H, Denker B. Renal pathophysiology. The essentials. Philadelphia. Lippincott Williams & Wilkins. 2007
5.- Macías Núñez J, Cameron S, Oreopoulos D. The aging kidney in health and disease. New York. Springer. 2008
6.- Musso CG. Potassium metabolism in patients with chronic kidney disease (CKD), Part I: patients not on dialysis (stages 3-4). Int Urol Nephrol. 2004;36:465-468.
7.- Musso CG, Reynaldi J, Vilas M, De Miguel R, Imperiali N, Algranati L. Fractional excretion of K, Na and Cl following furosemide infusion in healthy, young and very old people. Int Urol Nephrol. 2010 ;42:273-277
8.- Musso CG, Macías-Núñez JF. Dysfunction of the thick loop of Henle and senescence: from molecular biology to clinical geriatrics. Int Urol Nephrol. 2011;43:249-252
CORRESPONDENCE:
Carlos G. Musso
Sección Fisiología Clínica Renal. Servicio de Nefrología y Medio Interno.
Hospital Italiano de Buenos Aires.
Buenos Aires. Argentina
Email: carlos.musso @ hospitalitaliano.org.ar
