Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
URINARY INCONTINENCE: KNOWLEDGE, ATTITUDES, AND PREVALENCE AMONG OLDER ARGENTINE FEMALES.
Jauregui JR, MD. PhD.1, Fischer KB, MD.2, Musso CG, MD. PhD.1
1Geriatrician researcher. Biology of Aging Research Unit.
Hospital Italiano San Justo. San Justo. Argentina.
2Weill Cornell Medical College. New York. USA
profejauregui @ gmail.com
Rev Electron Biomed / Electron J Biomed 2013;1:18-24
Comment of the reviewer Dr. Alberto Enrique D'Ottavio. Professor and researcher. Facultad de Ciencias Médicas and Consejo de Investigaciones. Universidad Nacional de Rosario. Rosario, Argentina.
Comment of the reviewer Dra. María Cristina Tarrés, Professor and researcher. Facultad de Ciencias Médicas and Consejo de Investigaciones. Universidad Nacional de Rosario. Rosario. Argentina.
SUMMARY:
Objectives: This study aimed to investigate the knowledge and attitudes of Argentine women 65 years of age and older regarding urinary incontinence (UI).
Methods: A cross-sectional study of 238 community-dwelling Argentine women 65 years of age and older was conducted in San Justo, Argentina. Data were collected by in-person interviews.
Results: Regarding knowledge, 232 (97.5%) of the women surveyed were familiar with the term urinary incontinence, but 152 (63.9%) falsely believed that UI is a normal part of aging and 163 (68.5%) did not know about pelvic exercises or a surgical option to treat UI. A total of 106 (44.5%) women reported symptoms of UI.
Discussion: Older Argentine women are misinformed about UI. Interventions are necessary to increase their knowledge and healthcare seeking behaviors.
KEYWORDS: Argentine women. Urinary incontinence. Knowledge. Treatment. Geriatric.
RESUMEN:
Objetivo: Este estudio tuvo como objetivo investigar el conocimiento y las actitudes de las mujeres argentinas de edad mayor o igual a 65 años respecto de la incontinencia urinaria (IU).
Método: Se realizó un estudio transversal de 238 mujeres de edad mayor o igual a 65 años residentes de la ciudad de San Justo, Argentina. Los datos fueron recolectados a través de entrevistas personales.
Resultados: 232 de las mujeres entrevistadas (97.5%) estaban familiarizadas con el término de IU, pero 152 (68.5%) creían erróneamente que la IU era parte normal del envejecimiento y 163 (68.5%) no sabía acerca de los ejercicios pélvicos o una opción de tratamiento quirúrgico.
Conclusión: Las mujeres argentinas de edad mayor o igual a 65 años que habitan en la ciudad de San Justo, están mal informadas respecto de la IU, de modo que intervenciones son necesarias a fin de aumentar su conocimiento sobre el tema a fin de que tengan acceso a una mejor atención médica.
PALABRAS CLAVE: Mujeres argentinas. Incontinencia urinaria. Conocimiento. Tratamiento. Geriatría
INTRODUCTION
Urinary incontinence (UI) is a significant health problem that affects an estimated 200 million adult women worldwide1. Urinary incontinence, as defined by the International Continence Society Committee, is the "complaint of any involuntary leakage of urine"2. The effects of UI, especially amongst older women, can be debilitating physically, psychologically, and socially 3.
Studies have shown that most women with incontinence can be successfully treated by simple and effective methods4. However, the less women know about the symptoms, causes, and treatments of UI, the less likely they are to seek help5. Proper management of the condition by both healthcare professionals and community workers is dependent on women's attitudes and knowledge about UI4. It is likely that improving a woman's knowledge about UI will increase her healthcare seeking behaviors and the possibility of receiving effective treatment6.
Therefore, it is crucial to determine what women actually know about UI. Previous research has found Hispanic women to have a higher prevalence of UI compared to white, black, and Asian American women7. However, to the best of our knowledge, no data exist about UI knowledge and prevalence specific to older Argentine women.
The present study was conducted to answer the following questions: (1) What do community-dwelling Argentine women 65 years of age and older, regardless of their current UI status, know about UI? and (2) What is the prevalence of UI in a randomly selected sample of older Argentine women in our Hospital programmatic area?
MATERIAL AND METHODS.
Study Setting and Sample Assembly
This cross-sectional study was conducted between September 2009 and December 2009 at the Hospital Italiano (HI) de Buenos Aires in San Justo, Argentina. HI is a community-based, academically affiliated, out-patient and in-patient multi-specialty hospital. The out-patient clinic is staffed with primary care, geriatric, pediatric, and obstetric- gynecologist physicians. Occasionally, specialists see patients in this location. The clinic accommodates private patients, patients that are a part of an HI insurance plan, and patients with Obra Social, a form of insurance for Argentine workers.
Female patients attending the out-patient clinic coming for routine appointments were approached in the waiting corridor by the primary investigator (PI) and asked to participate in the study. Involvement was voluntary and the PI screened prospective women for eligibility. To be eligible, a female needed to be 65 years of age or older and speak Spanish. Women with known dementia or who appeared confused and/or disoriented were considered ineligible. Staff at HI deemed that the protocol did not require International Review Board approval. Verbal consent was obtained from all participants.
A total of 328 women were screened, 75 were ineligible mainly because they did not meet the age condition. Of the 253 women who met the eligibility criteria, eleven refused to take part in the survey with time being the most frequent excuse and four did not finish the survey because they were called to go see their doctor.
Survey Administration
All participants underwent an in-person interview conducted in the waiting area of the clinic. All encounters were carried out by the PI. On average, the interview took ten minutes (range 7-15 minutes). The PI explained to each woman that "the purpose of the study is to find out what you know about urinary incontinence, or the involuntary loss of urine."
Instrument
The research instrument was forward translated into Spanish by a fluent, native speaker and validated by Spanish speaking employees at HI. A pilot test for comprehension was conducted on 40 female HI patients who met the eligibility criteria. The established resulting survey was administered to subjects and the following data were collected:
Demographics
Information about participants' age and level of education was obtained.
Knowledge and Familiarity
To assess participants' knowledge about UI, a modified version of
the Incontinence Quiz (IQ), a tool established and validated by Branch and colleagues, was employed8. To the best of our knowledge, a validated Spanish language form of the IQ was not available. The IQ requires subjects to "agree", "disagree", or declare "I don't know" in response to a true or false statement about UI. For example: "Many over-the-counter medications can cause involuntary urine loss: agree, disagree, or I don't know"5. This format, when forward translated into Spanish, confused a pilot test group of female HI patients 65 years of age and older. It was determined that reframing the statement into a question would be a more familiar format for the women. The previous example was changed to: "Do you know if medications that you are able to buy over-the-counter can cause UI: yes they can cause UI, no they do not cause UI, or I don't know."
The resulting 12 question survey elicited data about participants' general familiarity with the topic of UI as well as their knowledge regarding the (a) causes of UI, (b) relationship of aging and UI, (c) doctor-patient communication about UI and (d) treatment options for UI. Subjects were also directly asked if they had UI. The type of UI - stress, urge, overflow, or mixed - was not differentiated in this study.
Prevalence
Women were asked the following question to assess if they had UI symptoms: "Have you ever lost urine during daily activities, at night, while coughing, sneezing, or laughing?" Answering "yes" to any of the above was considered a positive response. Participants who responded affirmatively were then asked: "Have you ever discussed your loss of urine with your primary care physician (PCP), gynecologist, a nurse or other healthcare professional?"
Statistical analysis
Data were analyzed using SNAP 10 professional. Surveys were coded to maintain anonymity. Demographic data were analyzed in order to characterize the study population. The frequencies of responses to each individual question were determined. Chi-squared tests were used to determine statistical associations between the independent and dependent variables. A P value of less than 0.05 was considered to be statistically significant.
The present study was approved by the Institutional Review Board and all participants provided written informed consent prior to performance the study interview to them.
RESULTS
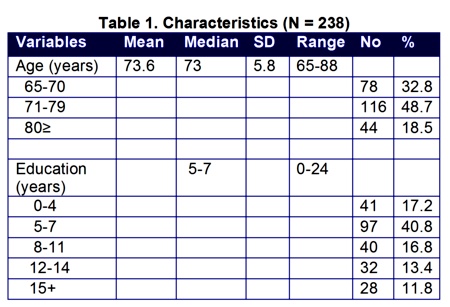
A total of 238 women enrolled in the study. Table 1 describes the demographic characteristics of the sample. Mean age was 73.6 ± 5.8 years and median amount of education was 5 - 7 years.
The participants' knowledge of and familiarity with UI are shown in Table 2. Almost all women, (97.5%) women were acquainted with the term UI. More than half of those surveyed could identify at least one women who had UI as well as spoke about the problem to their friends.
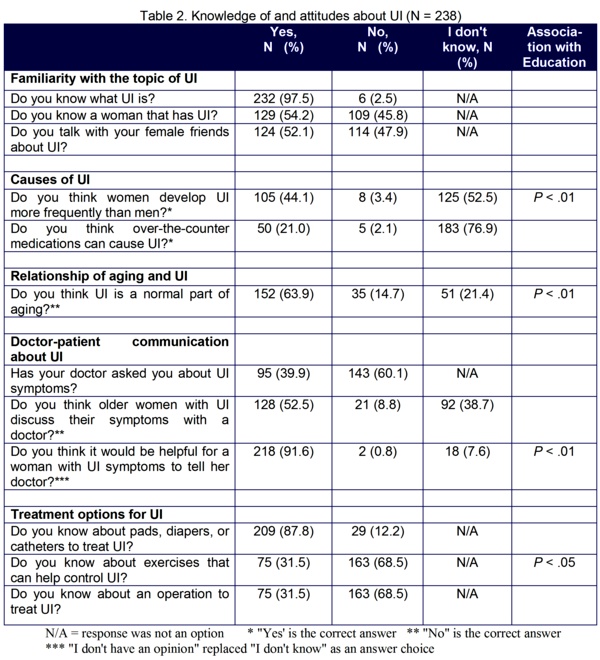
A large number of women were uninformed about the causes of UI: 182 (76.8%) did not know that over-the-counter medications can cause symptoms. When asked about the frequency of UI in men and women, 125 (52.5%) did not know if women experience UI more frequently than men, 8 (3.4%) thought that men and women develop UI at equal rates, and 105 (44.1%) accurately knew that more women suffer from UI than men. The association between years of education and knowledge about the frequency of UI in women and men was statistically significant (P<.01): women with more education were more likely to know that women develop UI more than men.
Women were misinformed about the relationship between aging and UI. A large number of women, 152 (63.9%), incorrectly thought that UI is a normal part of the aging process. It is noteworthy that 78.6% of women with the highest level of education (15+ years) believed UI was a normal part of aging compared to 41.5% of women with the lowest level of education (0-4 years). The association between believing that UI is a normal part of the aging process and completed years of education was statistically significant (P<.01): the more years of education a woman had completed the more likely she was to think that UI is a normal part of aging.
A majority of women, 217 (91.6%), accurately believed that it would be helpful for a woman with UI to discuss this condition with a doctor. The association between level of education and beliefs about telling the doctor about UI was statistically significant (P<.01): women with more years of education were more likely to know that sharing UI symptoms with a physician would be helpful. There were 143 (60.3%) subjects who had not been asked by their PCP's about UI symptoms.
Within the sample, 87.8% knew of pads, adult diapers, and catheters to treat UI. However, 68.5% of women did not know about pelvic exercises or a surgical option to treat UI. The association between level of education and knowledge of pelvic exercises was statistically significant (P<.05): women with more education were more likely to know of these exercises.
Prevalence data varied depending on how the question was solicited. When asked to self-identify as having UI, 58 (24.4%) women acknowledged suffering from the condition. However, when the study population was specifically asked about UI symptoms - such as urine loss during the day, night, while coughing, sneezing, or laughing - a larger group, 106 (44.5%), identified as having UI. Many participants, 46 (43.4%), who reported having UI symptoms did not consult a healthcare provider.
DISCUSSION
The purpose of this cross-sectional study was to determine what Argentine women 65 years of age and older know about UI and to establish the prevalence of UI in this population. Results for the 238 women studied showed that they were misinformed about the specific details (causes, aging, treatments, etc.) of UI. The information gleaned from this study elucidates the misconceptions that older Argentine women have about UI. Healthcare providers can use this information to develop interventions targeted towards increasing and correcting older Argentine women's knowledge about UI with the goal of improving management and treatment of symptoms.
Most women in this study believed that UI is a normal part of the aging process (63.9%), a finding consistent with other studies on the same topic. Kang found a similar result (61%) in a study of Korean-American women using the IQ 5. Bush and colleagues, in a study of community-dwelling American minority and non-minority females, found that almost 50% believed UI to be a normal part of aging or childbirth9. Because of a series of physical, psychological, and functional changes that are associated with aging, the prevalence of UI increases with age; however, UI is not the result of normal aging5. Ouslander reported that UI in a geriatric population can be a "manifestation of a subacute or reversible process within or outside of the lower urinary tract."10. Educating older Argentine women about this fact, through either community educational programs or physician-initiated discussions, can correct their view that UI is an inevitable part of aging and will hopefully lead to more successful treatment of UI and the underlying process(es).
Interestingly, in the current study, 78.6% of the highest educated (15+ years) women believed that UI was a normal part of aging. This demonstrates that even educated women are frequently misinformed, consistent with results from previous studies11. Accurate UI information must be provided to all patients, regardless of their education status. Physicians should not assume that more highly educated women are better informed about UI because there is a clear gap between lay and medical knowledge11.
Argentine women, as compared to women in other studies, are less knowledgeable about behavioral therapies that can be employed to treat UI. Among Korean-American women, 67% knew of exercises to help control UI compared with just 31.5% of Argentine women in the current study. Kang noted that Korean-American women were more knowledgeable about pelvic exercises compared to populations in other studies and attributed this finding to television programs and Korean language health magazines that educated Korean women about exercises they could do to decrease the effects of UI5. Hagglund and colleagues reported that women in their study might have been influenced to seek help for UI by reading magazine advertisements and/or watching television programs4.
Using similar media, targeted to older Argentine woman, can help to increase their UI knowledge and correct their misconceptions. Public service announcements on Spanish TV and radio stations or advertisements in magazines should (a) tell women that UI is a real and common medical condition that is not a normal part of aging, (b) inform women that there are simple and effective treatments available and that their symptoms can worsen and lead to functional decline when left untreated, (c) provide information about causes such as over-the-counter medicines and possible underlying or reversible disorders, and (d) encourage females to seek treatment from a healthcare professional. Providing this same information on posters and brochures at senior centers as well as adult living facilities is another method to enlighten, educate, and empower women. This education, supplemented with information provided by healthcare workers, can help to increase UI knowledge and change women's attitudes about UI.
The prevalence data generated in this study varied based on the definition of UI used in the question. A higher prevalence, an almost two-fold increase to 44.5%, was found when women were asked to identify based on symptoms as compared to simply stating that they had UI. This finding is consistent with other research. Hagglund and colleagues reported that when wide definitions of UI were used, a larger number of women, including those with only minor symptoms, identified as having the condition4. Thus, PCP's when assessing for UI, should use broad questions to ensure capturing those experiencing only minor symptoms as well. Knowing that UI can be the manifestation of a variety of processes, it is important to identify women experiencing even minor UI symptoms to treat both the condition and a potentially harmful underlying cause.
Consistent with these findings, a larger group of younger women (those less than 73 years of age) identified as having UI when the question used a wider definition that included symptoms. It is likely that these "younger" women perceived UI as a neurological or senile disorder and did not initially self identify as suffering from this condition despite having obvious symptoms 11. Because proper management depends on a woman's knowledge of UI, it is imperative that females are accurately educated about UI and its ability to affect women of all ages.
Although 91.6% of women surveyed believed it would be helpful to tell a doctor about one's UI symptoms, only 43.4% of those with UI symptoms actually sought out medical advice for this problem. This finding is consistent with previous research. Hsieh and colleagues found that among 1,514 Taiwanese women aged 60 years and older, 84.6% would tell a doctor if they had UI, but only 30.3% actually spoke to a physician3. Less than 20% of women in Finland and only 28.2% of European women sought out treatment as well12.
Some study limitations merit consideration. First, women were interviewed in a crowded waiting area where complete privacy was not feasible. As a result, it is possible that the women were not being completely truthful in their responses. Second, the sample population was small which potentially limits the ability to generalize the results to all older Argentine females.
It is clear that educational programs, both at the community and healthcare-provider level, need to be implemented to increase UI knowledge in older Argentine females. A useful follow-up study would be one conducted in the same sample population of women that assesses UI knowledge after the sample group has been privy to educational materials. Healthcare workers that develop and implement UI educational programs designed to increase knowledge will lead likely see a rise in help-seeking behavior among older Argentine women with UI.
CONCLUSIONS
Argentine women 65 years of age and older are poorly informed about UI. Misconceptions and a lack of knowledge lead to the under-treatment of UI symptoms. Providing accurate information to women is imperative to ensure the proper treatment of this disorder.
Education about UI by individual physicians as well as at the community level can dramatically improve the quality of life for older Argentine women suffering from UI. Findings from this study provide important data specific to Argentine women. Healthcare providers and community workers that interact with this population can design targeted educational materials aimed to increase UI information based on what this study has established as the current level of knowledge.
ACKNOWLEDGEMENTS
The authors thank the Argentine female patients and the wonderful nursing staff at the Hospital Italiano de Buenos Aires. The authors also thank Weill Cornell Medical College Professors Drs. Cary Reid and Sanchita Das for their continued support and contributions to this work.
CONFLICT OF INTEREST
The authors of this paper declare that there are not conflicts of interests.
REFERENCES
1.- Sampselle CM, Palmer MH, Boyington AR, O'Dell KK, Wooldridge L. Prevention of urinary incontinence in adults: population-based strategies. Nurs Res. 2004.53:S61-7.
2.- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology.2003. 61:37-49.
3.- Hsieh CH, Su TH, Chang ST, Lin SH, Lee MC, Lee MY. Prevalence of and attitude toward urinary incontinence in postmenopausal women. Int J Gynaecol Obstet. 2008. 100:171-174.
4.- Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Reasons why women with long-term urinary incontinence do not seek professional help: a cross-sectional population-based cohort study. Int Urogynecol J Pelvic Floor Dysfunct .2003.14:296-304
5.- Kang, Y. Knowledge and attitudes about urinary incontinence among community-dwelling Korean American women. J Wound Ostomy Continence Nurs .2009. 36:194-199.
6.- Kubik, K., L. Blackwell, and M. Heit. Does socioeconomic status explain racial differences in urinary incontinence knowledge? Am J Obstet Gynecol 2004. 191:188-193.
7.- Thom DH, van den Eeden SK, Ragins AI, Wassel-Fyr C, Vittinghof E, Subak LL, Brown JS. Differences in prevalence of urinary incontinence by race/ethnicity. J Urol. 2006.175:259-264.
8.- Caljouw MA, den Elzen WP, Cools HJ, Gussekloo J. Predictive factors of urinary tract infections among the oldest old in the general population. A population-based prospective follow-up study. BMC Med. 2011. 16;9:57
9.- Bush TA, Castellucci DT, Phillips C. Exploring women's beliefs regarding urinary incontinence. Urol Nurs. 2001. 21:211-218.
10.- Kashyap M, Tu LM, Tannenbaum C. Prevalence of commonly prescribed medications potentially contributing to urinary symptoms in a cohort of older patients seeking care for incontinence. BMC Geriatr. 2013. 10;13(1):57.
11.- Rizk DE, El-Safty MM. Female pelvic floor dysfunction in the Middle East: a tale of three factors--culture, religion and socialization of health role stereotypes. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:436-438.
12.- Khandelwal C, Kistler C. Diagnosis of urinary incontinence. Am Fam Physician. 2013. 15;87(8):543-50
CORRESPONDENCE:
JR Jauregui MD, PhD
Biology of Aging Research Unit
Hospital Italiano de san Justo
Av. Juan D. Perón 2231
1754 AZK - San Justo
Provincia de Buenos Aires - Argentina
profejauregui @ gmail.com
