Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
Letters to the Editor / Cartas al Editor
TARGETOID-LIKE CUTANEOUS AGGRESSIVE EPIDERMOTROPIC CD8+ CYTOTOXIC T-CELL LYMPHOMA
David A. De Luca1, Gianina M. Alcalá Cepeda1, Ana C. Torre1,
Hernán García Rivello2, Paula A Enz1
1Servicio de Dermatología, 2Servicio de Anatomía Patológica.
Hospital Italiano de Buenos Aires, Argentina.
Email: enzpaula @ gmail.com
Rev Electron Biomed / Electron J Biomed 2016;2:52-55
To the Editor:
Primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma (PCAE-TCL) is a rare disease that represents less than 1% of the primary skin lymphomas1.
Due to its aggressive nature, it can spread rapidly to the lung, central nervous system and oral cavity, without affecting the lymph nodes, with an average survival of 32 months.
Classified as a provisional entity by the World Health Organization - European Organization for Research and Treatment of Cancer (WHO-EORTC 2005), PCAE-TCL has a poor prognosis and blood dissemination to lungs, testis, central nervous system and oral cavity are the rule, although lymph nodes are often spared2-4.
We report the case of a 73-year-old Caucasian male patient with type 2 diabetes mellitus, dyslipidemia and right carotid endarterectomy, who was referred to our hospital with a one-year history of asymptomatic skin lesions.
On clinical examination he showed multiple round pinkish and purple, targetoid-like and ulcerated, crusted plaques and nodules from 1 to 10 cm in limbs, trunk and face (Figure 1). In addition, he presented 8mm-erythematous macules around the urinary meatus and on the hard palate.
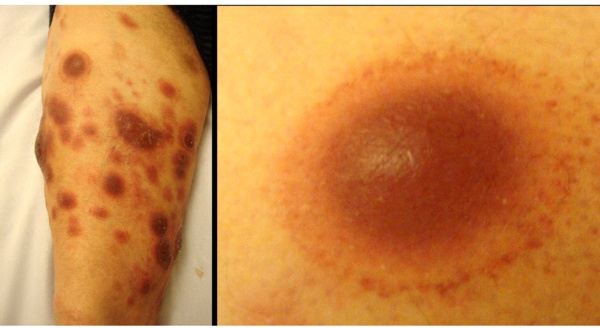
Figure 1: Multiple round pinkish and purple, targetoid-like, crusted plaques and nodules in limbs.
Blood test and whole-body CT scan were normal and HIV, HBV and HCV were negative. Reactive changes without atypia were found on bone marrow aspiration and its biopsy. The histopathology of an excisional biopsy of a lesion showed a cohesive sheet of large and pleomorphic lymphoid cells with a high mitotic index, infiltrating epidermis, dermis and subcutaneous tissue and angiocentricity.
The immunohistochemistry of the skin revealed lymphoid cells CD3+, CD4-, CD8+, CD20-, CD30-, CD56- and the monoclonal T-cell receptor beta-chain gene rearrangement of TCR by PCR was positive (Figure 2). The flow cytometry of the skin showed CD2+, CD4-, CD5+, CD7-, CD8+, TCR  /
/ + and TCR
+ and TCR  /
/ .
.
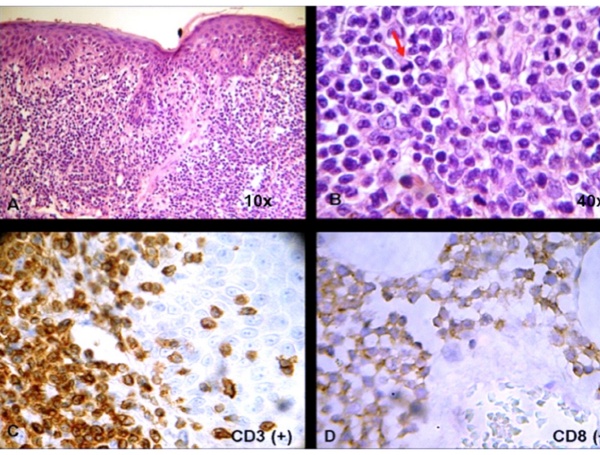
Figure 2: (a) H&E 10x - Cohesive sheet of lymphoid cells infiltrating epidermis, dermis and subcutaneous tissue and angiocentricity. (b) H&E 40x - Large and pleomorphic lymphoid cells with a high mitotic index (red arrow). (c) Skin immunohistochemistry reveals CD3+ and (d) CD8+ lymphoid cells.
The diagnosis of PCAE-TCL was confirmed and he received cyclophosphamide, doxorubicin, vincristine and prednisone with partial remission of the skin lesions. After completing two cycles of chemotherapy, the patient died of cardiac causes three months after the diagnosis, without evidence of extracutaneous disease.
PCAE-TCL is a rare and clinical heterogeneous lymphoma in adults with a predominance in male5.The clinical picture differs in each case, but eruptive papules, hyperkeratotic or ulcerated nodules and tumors with crust and necrosis are often the rule4,5.
Unlike mycosis fungoides, skin lesions in PCAE-TCL affect sun-exposed skin and mucous membranes.
We describe a patient with an atypical targetoid-like plaques and nodules due to the hemorrhagic component, along with red macules in mouth and penis without systemic disease. Despite the clinical picture or remission to chemotherapy, progressive disease with a median survival from 12 months to 36 months was described2-6.
Recently, a patient with PCAE-TCL achieved complete remission with an allogenic stem cell transplantation and he was 36 month free of disease7.
Conclusion: the inspection of skin lesions and their histopathological and immunohistochemical examination are crucial for primary cutaneous T-cell lymphoma diagnoses.
REFERENCES
-
1. Gormley RH, Hess SD, Anand D, Junkins-Hopkins J, Rook AH, Kim EJ. Primary cutaneous aggressive epidermotropic CD8+ T-cell lymphoma. J Am Acad Dermatol 2010;62:300-307.
2.- Willemze R, Jaffe ES, Burg G et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-3785.
3.- Slater DN. The new World Health Organization-European Organization for Research and Treatment of Cancer classification for cutaneous lymphomas: a practical marriage of two giants. Br J Dermatol 2005;153:874-880.
4.- Berti E, Tomasini D, Vermeer MH, Meijer CJ, Alessi E, Willemze R. Primary cutaneous CD8-positive epidermotropic cytotoxic T cell lymphomas. A distinct clinicopathological entity with an aggressive clinical behavior. Am J Pathol 1999;155:483-492.
5.- Robson A, Assaf C, Bagot M, et al. Aggressive epidermotropic cutaneous CD8+ lymphoma: a cutaneous lymphoma with distinct clinical and pathological features. Report of an EORTC Cutaneous Lymphoma Task Force Workshop. Histopathology 2015;67:425-441.
6.- Nofal A, Abdel-Mawla MY, Assaf M, Salah E, Abd-Elazim H. Primary cutaneous aggressive epidermotropic CD8+ T cell lymphoma: a diagnostic and therapeutic challenge. Int J Dermatol 2014;53:76-81.
7.- Wehkamp U, Glaeser D, Oschiles I, Hilgendorf I, Klapper W, Wichenthal M. Successful stem cell transplantation in a patient with primary cutaneous aggressive cytotoxic epidermotropic CD8+ T-cell lymphoma. Br J Dermatol 2015;173:869-871.
CORRESPONDENCE:
Paula Enz
Servicio de Dermatología
Hospital Italiano de Buenos Aires, Argentina
Buenos Aires.
Argentina
Email: enzpaula @ gmail.com
