Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
- Hypertension is an average of values of systolic arterial pressure = 140 mm Hg and/or an average of values of diastolic arterial pressure =90 mm Hg obtained in the arm with the patient seated.
- The isolated systolic hypertension was defined as values average of systolic arterial pressure = 140 mm Hg, with normal diastolic blood pressure17.
- Early nephrology referral (ER) was defined as a first nephrology visit = 4 months prior to initiation of dialysis.
- Late nephrology referral (LR) as first nephrology visit =4 months prior to initiation of dialysis7-10.
- All of them received erythropoietin treatment subcutaneously at an initial dosage of 30 U/kg/dose three times a week. The dosage was increased according to response, or reduced if the hematocrit was =36%. Iron Dextran was administered intravenously at 100 mg/week and at 50 mg/week there after and oral rute was given as needed to maintain transferring saturation >20%. They were evaluated at starting, at around 12 weeks (expected time to reach target hemoglobin of 11 g/dL).
- Hypoalbuminemia was defined as serum albumin <3.5 g/dl.
- Late initiation of dialysis was defined as initiation of dialysis at a predicted GFR <5 ml/min per 1.73 m2. (Creatinine > 7 mg/dl ).
- Clinical and laboratory data were obtained from the patient records and electronic databases of the office records of the dialysis Unit. Using a standardized form, age, gender, race, insurance status, cause of ESRD, laboratory values obtained within 24 h before initiation of dialysis, pre-ESRD erythropoietin use, presence and type of permanent access used for the first dialysis, initial dialysis modality, predicted GFR, and index of individual disease severity at the initiation of dialysis were recorded for each patient. Predicted GFR was calculated from the equation derived from the Modification of Diet in Renal Disease Study, and is based on age, gender, race, and levels of blood urea nitrogen, serum albumin, and serum Creatinine.
- Data were collected and analyzed using the software "Epi-Info" (version 6.04 fr).
- In every hemodialysis we did to the patients:
- Predialysis weight estimation.
- Predialysis BP measures.
- BP hourly during the 3h haemodialysis.
- Postdialysis BP measures.
- Reweighed again at the end of the dialysis.
- Patients were dialyzed with Hemodialysis Machine Fressenuis 4008-H and volumetric dialyser, bicarbonate buffer based dialysate, blood flow 300-350 ml/min, dialysate flow 500 ml/min, ktv 1.34 ± 0.12. All patients were dialyzed three times a week, each session lasting 3-4 hours. Polysulphone hollow fibers dialyser (1.8 m2), were used.
- Patients were included when they were on maintenance HD and using a dual-lumen central venous catheters (CVC), located in the Internal Jugular vein (IJV), Subclavia veins and Femoral veins also were hemodynamically stable (defined as stable BP on dialysis without the need for saline bolus for the previous 2 wk).
- Qat: According to the World Health Organization (WHO)18, qat grows on an evergreen (Catha edulis), a slender, straight tree found in mountainous terrain and reaches a height of perhaps two or three meters in the Yemen. In Africa it can be four or five times as tall. The leaves of the qat plant contain alkaloids structurally related to amphetamine and they are currently chewed daily by a high proportion of the adult population in Yemen for the resulting pleasant mild stimulant action19. The pleasurable central stimulant properties of qat are commonly believed to improve work capacity, are used on journeys and by students preparing for examinations and to counteract fatigue15-16.
STUDY OF CHRONIC RENAL FAILURE IN MILITARY HOSPITAL SANA’A. YEMEN.
*Jose Luis Rodriguez, **Roberto Arteaga Crespo.
*Specialist in Nephrology. **Specialist in Internal Medicine
Military Hospital. Sana’a. Republic of Yemen
jluisr5106 @ yahoo.es
Rev Electron Biomed / Electron J Biomed 2008;2:27-38
Comment of the reviewer Carlos Musso MD. PhD. Department of Nephrology. Hospital Italiano. Buenos Aires. Argentina
Comment of the reviewer Basilia González MD. PhD. Department of Nephrology. Hospital General Yagüe. Burgos. España
ABSTRACT:
Chronic Renal Failure (CRF) is a major public health problem. Early diagnosis and treatment are basic for its prognosis, and it will be fundamental for the future necessity of substitutive renal treatment. For this purpose, determining the etiology of CRF may be helpful.
This study was conducted in the Nephrology Department at the Central Military Hospital in Sana’a, Yemen from 2004 to 2007; to determine the etiology of CRF in 334 patients (211 men and 123 women) on regular hemodialysis.
The Hypertensive Nephropathies (24%) was the commonest cause of CRF. Diabetic Nephropathies (20%), Obstructive Nephropathy (16%), Chronic Pyelonephritis, Glomerulonephritis, Polycystic Kidney, Schistosomiasis (Bilharzias) were less common. There were more men than women (63% vs. 37%, respectively). The mean age range of the patients was 42 years old. At study entry, 86 (29%) were dialyzing via native Artery Venous Fistula (AVF) and 11 (4.7%) through a synthetic graft. The Temporary Catheter was the most common form of vascular access used in 272 (81%) patients and AVF the second most frequent (26%). The mortality during this period was 22.9%, being the Cardiovascular Disease the main cause of death (56%), followed by Septicemia (18%). Other causes of death included Pulmonary Infection and Cirrhosis. Hypertension, late referral, smoking and Qats were the commonest co-morbid causes.
According to our study we would like to include the habit of chewing Qats as a risk factor to progression of End-Stage Renal Disease (ESRD) in patients with CRF.
Keywords: Renal replacement therapy. Maintenance haemodialysis. Chronic renal failure (CRF). End-stage renal disease (ESRD).
RESUMEN: ESTUDIO DE LA INSUFICIENCIA RENAL CRÓNICA EN EL HOSPITAL MILITAR DE SANA’A. YEMEN.
La Insuficiencia renal crónica (IRC) es un importante problema de Salud Pública. El diagnóstico precoz y el tratamiento son básicos para su pronóstico, y fundamentales para la futura necesidad de tratamiento renal sustitutivo. A tal efecto, puede ser de utilidad determinar la etiología de la IRC.
Este estudio fue realizado para determinar la etiología de la IRC en 334 pacientes (211 hombres y 123 mujeres) en hemodiálisis periódica, se llevó a cabo en el Departamento de Nefrología del Hospital Militar Central en Sana'a, Yemen, entre los años 2004 y 2007.
La nefropatía hipertensiva (24%) fue la causa más común de IRC. La nefropatía diabética (20%), la nefropatía obstructiva (16%), la pielonefritis crónica, la glomerulonefritis, la enfermedad renal poliquística y la esquistosomiasis (Bilharzias) fueron mucho menos frecuentes. Hubo más hombres que mujeres (63% vs 37%, respectivamente). La media de edad de los pacientes fue de 42 años de edad. En la entrada de estudio, 86 (29%) fueron dializados a través de la fístula arteria venosa (AVF) y 11 (4,7%) a través de un injerto sintético. El catéter temporal fue la forma más común de acceso vascular, siendo utilizado en 272 (81%) pacientes y AVF la segunda más frecuente (26%). La mortalidad durante este período fue del 22,9%, siendo las enfermedades cardiovasculares la principal causa de muerte (56%), seguida de septicemia (18%). Otras causas de muerte incluyen la infección pulmonar y cirrosis. La hipertensión arterial, la remisión tardía, el consumo de tabaco y Qats fueron las causas de comorbilidad más comunes.
Según los datos de nuestro estudio, debería incluirse el hábito de mascar Qats como un factor de riesgo para la progresión de la enfermedad renal terminal (ESRD) en pacientes con IRC.
Palabras clave: Terapia de reemplazo renal. Hemodiálisis periodica. Insuficiencia renal crónica (IRC). Enfermedad renal terminal (ESRD).
INTRODUCTION
The advances in renal replacement therapy have been remarkable taking end-stage renal disease (ESRD) from an invariably fatal disease in the first half of the last century to a disease with mortality rate of about 20% - 25% per year1-2. This success is not complete in spite of the recent improvements in dialysis and dialysis prescription, treatment of anemia, hypertension and bone disease. The population of ESRD is growing fast; mortality is still unacceptably high, frequent hospitalization is required; sexual function is unsatisfactory and return to work is infrequent1-3.
There is a large population on dialysis world wide. The social and economic consequences of Chronic Renal Failure (CRF) are considerable. The Epidemiologic research has demonstrated that there is an increment in incidence, prevalence and complications of this disease2,4-5.
It is an important increased health problem in the world and also in Yemen1,3,6. The progression of ESRD has caused a yearly exponential rise in new patients, which require renal replacement, such as dialysis or renal transplant (from 7% to 10%, depending of the country)3-4. One big reason of that problem is the aging of the world’s population and the fact that they are living at present with different diseases responsible for early deaths. That is the case of Diabetes Mellitus and Hypertension, the two main causes of CRF. As people live more years with these conditions, they are more likely to develop ESRD or the point when a person needs dialysis or a kidney transplant to survive. In addition to the ethic, economic, and social effects on health services and society, this creates significant human suffering for the patient and his family1,4,6.
Several studies have examined the possible association between late referral to a nephrologists and mortality on maintenance dialysis in patients with CRF7-8. Other investigations have measured the effect of late referral on outcomes such as timely vascular access creation9-10, modality choice for renal replacement therapy and technique survival and health care costs5.
Hypertension, Diabetes Mellitus, Anemia, salt intake and hyperlipidemia have been identified as risk factors of CRF. They may play a great role in those patients11-12.
In Yemen Chewing Qat is a purely social (but gender-separate) event13-16. Many of our patients practice this habit, then we would like to consider it as one of the risks factor or as a direct modulator of the progression of CRF and their influences in its complications and mortality in haemodialyzed patients.
In the Dialysis Service of General Military Hospital in Sanaa, Yemen we identified an unacceptably high rate of inadequately prepared patients starting dialysis. In addition clinical practice guidelines and research-based recommendations are not used correctly.
The objective of the present study was to know the characteristics and to identify the associated risks factors in the study group of patients in our units of dialysis in Sana’a, Republic of Yemen.
MATERIALS AND METHODS:
We made a retrospective, descriptive study in order to determine the clinical and paraclinical features from the patients at the moment of entrance to dialytic therapy at Dialysis Unit of Military Hospital Sana’a Yemen, for regular dialysis. The medical records of 334 ESRD patients were treated during three years (from January 2004 to June 2007). We retrospectively evaluated the risk factor and mortality of those patients. In addition the causes of CRF, clinical and characteristics and comorbid conditions. Through clinical histories review we obtained: gender, age, presenting symptoms, past history etc.
The inclusions criteria used were:
-
1) Patients with ESRD. (Creatinine > 7 mg/dl)
2) Underwent haemodialysis therapy for more than 3 months.
3) Never having received a renal transplant.
4) 12 or more years of age.
5) Agreed to participate in the study by signing an informed consent.
Definitions:
Early clinical observations had suggested that qat has amphetamine-like properties, and subsequent chemical analysis confirmed that the fresh leaves contain alkaloids such as cathine and cathinone, the latter being structurally related and pharmacologically similar to amphetamine. Qat leaves also contain considerable amounts of tannins (7–14% in dried material), vitamins, minerals and flavonoids. Cathinone is currently believed to be the main active ingredient in fresh qat leaves20. Use of qat may lead to chronic hypertension which upon abstinence from the drug, can change into a transient hypotensive state18.
Comorbid Conditions: we included as Comorbid Conditions the presence of cardiovascular diseases, diabetes mellitus, liver cirrhosis, late referral, showing Qat and smoking in patients with CRF.
The dialysis access in use at the time of study initiation was recorded as one of four categories: native arteriovenous fistula (AVF) (a surgically created anastamosis between artery and vein to create a robust port of access for haemodialysis); synthetic vascular access graft and temporary catheters. (Non-tunneled central venous catheter).
All patients had been on hemodialysis for 4–15 years (mean, 8 years) and had undergone multiple prior catheter access procedures and multiple failed permanent access procedures.
RESULTS:
The study included 334 patients under regular hemodialysis therapy, 211 (63%) males and 123 (37%) females. The mean age was 42 years old (range from 12-85 years). The principal causes of ESRD were Hypertension with 80 (23.9%) individuals and Diabetes Mellitus with 65 (19.5%).The other causes were distributed in Obstructive Nephropathy, Pyelonephritis, Glomerulonephretis, Polycystic Kidney Disease, Schistosoma and Unknown Causes (table 1).
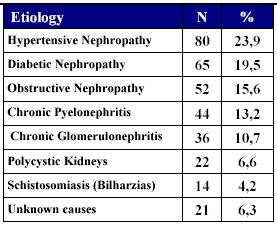
TABLE 1. PRINCIPAL ETIOLOGIES
All causes of ERSD were more frequent in male than female except Chronic Pyelonephritis that was common in female (table 2).
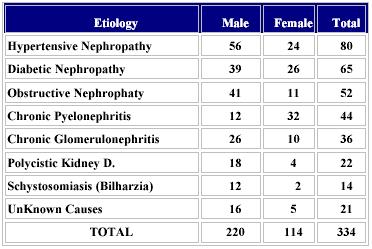
TABLE 2. ETIOLOGY AND SEX
Distribution according to age group, (table 3): Most of the patients (198) were 40 or more years olds, and the most frequent group affected was 40-55 years.
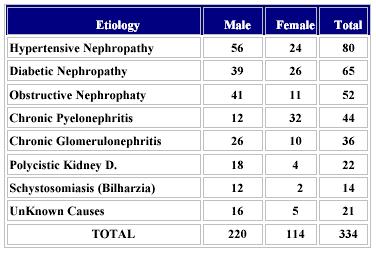
TABLE 3. DISTRIBUTION ACCORDING TO AGE
Age mean = 42 years Age range = 12-85 years
Table 4 represented clinical characteristic, biological parameters and procedures of patients: On admission only 97 (29.0%) cases had a vascular access and many of then presented serum creatinine > 9 mg/dl (87.7%),serum albumin <2g/dl (80.3%) and serum hemoglobin <9 g/dl (77.8%). After Admission we needed to implanted a temporal catheter in 237 patients, the most used vein was internal jugular vein (228 cases). We perform 162 AVF that represented the 68.3% of the cases.
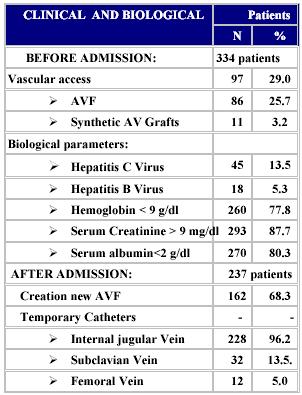
TABLE 4. CLINICAL CHARACTERISTICS, BIOLOGICAL PARAMETRES AND PROCEDURES
The predominant comorbid conditions were Hypertension with 193 (57.8%) cases, follow by Liver Cirrhosis and Diabetes Mellitus. Other important risk factors found in our study were: Late Referral (51.8%), Smoking (50.6%) and Qat (40.0 %). Table 5.
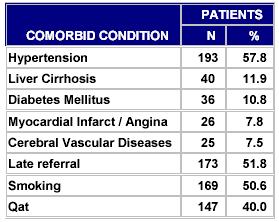
TABLE 5. COMORBID CONDITIONS. N = 334
Table 6 shows a total mortality of 86 (25.7%) patients. The primaries causes of death were Heart Failure, represented by 20 (23.3%) cases and Septicemias with 18 (20.9%) patients.
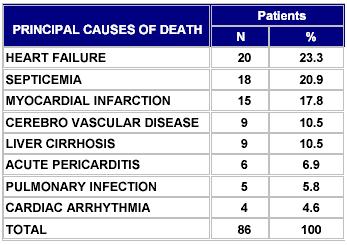
TABLE 6. DISTRIBUTION BY CAUSES OF DEATH
DISCUSSION:
During the last years the hemodialysis treatment has changed thanks to the marked technological advances, remarkably improving the quality of life of patients submissive this treatment21. Although hemodialysis effectively contributes to long-term survival, morbidity and mortality of dialysis patients remains high, especially morbidity and mortality due to cardiovascular diseases22-23. Only 32% to 33% of patients on hemodialysis survive to the fifth years of treatment, whereas 70% of patients who have kidney transplants are alive after 5 years4-5,23. Successful renal transplantation is considered the preferred and most cost effective method of treating patients with ESRD24-25.
The main cause of ESRD in our study was Arterial Hypertension, those finding differs to the cause of ESRD reported before from other authors26-29. However, our study showed that few patients had Diabetes Mellitus in comparison with developed countries that reported 25-35% prevalence of DM in the dialysis population30-31. This is not easy to explain. It is likely that in Yemen Diabetes Mellitus is under Diagnosed32.
We found a high frequency of hypertension correlative with habit to chew Qats17-19.The World Health Organization (WHO) considers Qats to have amphetamine-like properties, and categorizes it as a separate drug group in which it is the sole member. In its analysis of Qats, the WHO contends that chronic Qats-chewing can cause hypertension in young adults, with a spontaneous regression once consumption is stopped18.
Hypertension has been linked to the progression of CRF since the pioneering days of Richard Bright in the 19th century to Volhard and Farr (33,34).More recently, a large body of evidence has suggested that the progression of CRF is accelerated by raised systemic blood pressure35-38. This is likely to be due to the susceptibility of their glomeruli to systemic hypertension, as remnant glomeruli are poorly autoregulated and therefore allow the unopposed transmission of systemic hypertension to their capillary bed. The ensuing glomerular capillary hypertension accelerates the development of glomerulosclerosis39-41.
In our study 15.8% patients had Obstructive Nephropathy, secondary the presence of Kidney Stones, this percentage is high compared with the 3% reported from other countries42-43, this result we found is in relation to poor water quality in this region. Most recent epidemiological studies explain those results and say that water hardness ranging between the values commonly reported for drinking water is a significant factor in urolithiasis44-45.
The results of our study are the same that those support the argument that IJV is superior to the SCV as the access route46-47. Subclavian veins should not be use unless the jugular veins are inaccessible, avoid the subclavian vein if possible48-51.
We found on admission only 29% of patients with native AVF functioning as the first permanent access and synthetic Av Graft in few cases. In our Study was necessary to insert 272 new catheter, this outcome was related with late referral to our Nephrology Service.
Late referral of patients has been a constant problem in Unit Dialysis Departments52-54. In our study many patients were referred late, associated with suboptimal ESRD. Late referral usually conduces to emergency dialysis for acute complications such as fluid overload, arterial hypertension, pericarditis or gastro-intestinal complications of uraemia. Recent reports from several countries clearly indicate that approximately 30-50% of patients are referred too late to a nephrology unit10,54.
In contrast, early referral to a nephrologist allows to start a dialysis plan with treatment modality choice and permanent vascular access creation55-56.
Hepatitis C Virus (HCV) infection is frequent in patients undergoing chronic hemodialysis, with prevalence between 8 and 10%, and there is a particular concern because of the high risk for chronic liver disease, complications in renal transplantation, and death in those patients57-58.
This could be due to the non-adherence to the strict universal infection control measures and the unavailability of vaccines to prevent hepatitis C infection 59-60. Moreover, the increased facilities and advanced hemodialysis techniques have prolonged patients' survival which increased their risk of acquiring HCV.The extensive use of recombinant erythropoietin to correct renal anemia in HD patients resulted in a significant reduction in blood transfusions. However, previous studies have shown that de novo infections in single HD units may occur in the absence of other parenteral risk factors57. It has been suggested that infection could be transmitted from patient to patient in the hospital, and there is now indirect evidence that HCV infection occurs among HD patients during repeated dialysis procedures, but not through the equipment, probably due to procedural errors58.
We found high quantity of patients with hepatitis C positive virus but less than previous reported60. In addition those cases were associated with longer duration of dialysis, older age, previous surgery, and multiple blood transfusions. Those agree with previous reports59-60.
Qats and smoking, together with late referral and hypertension were the predominant causes of comorbidity. Over the last decades, more attention has been focuses on the potential nephrotoxicity of cigarette smoking61-62. Smoking as little as a single cigarette is associated with a rise in systemic blood pressure, direct renal hemodynamic effects leading to glomerular hyper filtration63-66.
We think that habit of chewing Qats has to consider as an important risk factor in the progression of ESRD in patients with CKD.
Despite improvements in dialysis care, the mortality of patients with ESRD in United States and Europe countries remains high, the reasons for this high mortality are probably related to the poor clinical conditions of patients at the beginning of the dialysis program and the association with comorbid factors67-71. The results of our study are consistent with those. In Summary, the morbidity and mortality of patients with ESRD are serious problems in Yemen as in the world.
REFERENCES
1- DuBose TD Jr. American Society of Nephrology Presidential Address 2006: Chronic Kidney Disease as a Public Health Threat--New Strategy for a Growing Problem. J Am Soc Nephrol. 2007; 18: 1038–1045.
2.- Hemmelgarn BR, Manns BJ, Zhang J, Tonelli M, Klarenbach S, Walsh M, Culleton BF. Association between multidisciplinary care and survival for elderly patients with chronic kidney disease. J Am Soc Nephrol. 2007;18:993-999.
3.- Jassal SV, Trpeski L, Zhu N, Fenton S, Hemmelgarn B. Changes in survival among elderly patients initiating dialysis from 1990 to 1999. CMAJ. 2007;177:1033-1038.
4.- Locatelli F, Marcelli D, Conte F, D’Amico M, Del Vecchio L, Limido A, Malberti F, Spotti D: Survival and development of cardiovascular disease by modality of treatment in patients with end-stage renal disease. J Am Soc Nephrol. 2001; 12: 2411–2417.
5.- Salonen T, Reina T, Oksa H et al. Cost analysis of renal replacement therapies in Finland. Am J Kidney Dis 2003; 42: 1228–1238.
6.- Mitra PK, Bradley JR. Chronic kidney disease in primary care. J R Soc Med. 2007; 100: 40–45.
7.- Tang SCW, Ho YW, Tang AWC et al. Delaying initiation of dialysis till symptomatic uraemia—is it too late? Nephrol Dial Transplant. 2007;22:1926-1932
8.- Winkelmayer WC, Owen WF. A Propensity Analysis of Late Versus Early Nephrologist Referral and Mortality on Dialysis J Am Soc Nephrol. 2003; 14:486-492
9.- Huisman RM. The deadly risk of late referral. Nephrol Dial Transplant. 2004; 19: 2175 -2180
10.- Kazmi WH, Obrador GT, Khan SS, Pereira BJ, Kausz AT. Late nephrology referral and mortality among patients with end-stage renal disease: a propensity score analysis. Nephrol Dial Transplant. 2004 ;19:1808-1814.
11.- Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med. 1997;14 Suppl 5:S1-85
12.- Ritz E, Rychlik I, Locatelli F, Halimi S, End-stage renal failure in type 2 diabetes: A medical catastrophe of worldwide dimensions. Am J Kidney Dis. 1999; 34: 795–808.
13.- Al-Amrani, M., The use of qat and its legal issue. Al-Irsahd Magazine, Sana’a. 1979
14.- Carapico S. Yemeni agriculture in transition. In P. Beaumont and K. McLachlan, eds. Agricultural Development in the Middle East. New York: John Wiley and Sons Ltd. 1985: 241–254
15.- Hassan NAGM, Gunaid AA, El Khally FMY, Murray-Lyon IM. The subjective effects of chewing qat leaves in human volunteers. Annals of Saudi Medicine 2003; 22: 34–37
16.- CYS, Qat in Yemen and in Yemeni Life (in Arabic). Center for Yemeni Studies, Sana’a, CYS, 1982: 341
17.- Klag MJ, Whelton PK, Randell BL, Neaton JD, Brancati FL, Ford CE, Shulman NB, Stamler J. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996; 334:13–18.
18.- Halbach H. Medical aspects of the chewing of khat leaves. Bulletin of the World Health Organization 1972;47:21–29
19.- Kalix P. Pharmacological properties of the stimulant khat. Pharmacol Ther. 1990; 48: 397–416
20.- Hes JP. [The use of Catha edulis among Yemenite Jews] Harefuah. 1970;78:283-284.
21.- European Renal Association-European Dialysis and Transplant Association. ERA-EDTA Registry 2004 Annual Report. Amsterdam, the Netherlands: Department of Medical Informatics, Academic Medical Center; 2006.
22.- Goodkin DA,Young EW, Kurokawa K et al. Mortality among hemodialysis patients in Europe, Japan, and the United States: case-mix effects. Am J Kidney Dis. 2004; 44: 16–21.
23.- Jungers P, Massy ZA, Nguyen-Khoa T, Choukroun G, Robino C, Fakhouri F, Touam M, Nguyen AT, Grünfeld JP: Longer duration of predialysis nephrological care is associated with improved long-term survival of dialysis patients. Nephrol Dial Transplant. 2001;16: 2357–2364, 2001.
24.- El-Nono IH, Al-Ba'adani TH, Ghilan AM, Asba NW, Al-Alimy GM, Al-Massani MM, Noman MA, Al-Shargabe S, Al-Mansour MM, Nassar MY. Adult-to-adult living related donor renal transplantation in Yemen: the first experience. Saudi J Kidney Dis Transpl. 2007;18:265-269.
25.- Collins AJ, Kasiske B, Herzog C, et al. Excerpts from the United States Renal Data System 2003 Annual Data Report: atlas of end-stage renal disease in the United States. Am J Kidney Dis. 2003;42(6 suppl 5):A5–A7.
26.- Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD. Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int 2003;63:793-808.
27.- Wright JT, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease. JAMA 2002;288:2421-2431
28.- Weber MJ. Natural history of hypertension. J Hypertension. Kidney Int 2003;21(suppl 6):S37-S46.
29.- Rodicio JL, Alcazar JM, Ruilope LM. Influence of converting enzyme inhibition on glomerular filtration rate and proteinuria. Kidney Int 1990; 38: 590-594.
30.- Molitch ME, DeFronzo RA, Franz MJ, Keane WF, Mogensen CE, Parving HH. American Diabetes Association. Diabetic nephropathy. Diabetes Care 2003;26(Suppl 1):S94–S98
31.- Finne P, Reunanen A, Stenman S, Groop PH, Gronhagen-Riska C. Incidence of end-stage renal disease in patients with type 1 diabetes. JAMA 2005;294:1782–1787
32.- Badheeb AM. Causes of Chronic Renal Failure in Hemodialysis Unit: A single center experience in Yemen. Saudi J Kidney Dis Transpl 2006;17:66-69.
33.- Dannenberg AL, Kannel WB: Remission of hypertension.The ‘natural’ history of blood pressure treatment in the Framingham Study. JAMA 1987;257:1477–1483.
34.- Foley RN, Parfrey PS, Sarnak MJ. Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol 1998; 9:S16-S23.
35.- Ruilope LM. Renal function and cardiovascular risk in hypertensive patients. J Hypertens. 2005; 23: 1787–1788.
36.- De Leeuw PW, Ruilope LM, Palmer CR, Brown MJ, Castaigne A, Mancia G, Rosenthal T, Wagener G. Clinical significance of renal function in hypertensive patients at high risk: Results from the INSIGHT trial. Arch Intern Med 2004;164: 2459–2464.
37.- Ruggenenti P, Schieppati A, Remuzzi G.Progression, remission, regression of chronic renal diseases. Lancet 2001; 357:1601–1608.
38.- Formica RN. CKD series: Delaying the progression of chronic kidney disease. Hosp Physician. 2003;43: 24–33.
39.- Jones CA. Hypertension and renal dysfunction: NHANES III. J Am Soc Nephrol. 2003;14: S71–S75.
41.- McClellan WM, Flanders WD. Risk factors for progressive chronic kidney disease. J. Am Soc Nephrol. 2003;14: S65–S70.
42.- Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am. J. Kidney Dis. 2003;41:1–12.
43.- Levey A S, Coresh J, Balk E et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann. Intern. Med. 2003;139: pp. 137–147.
44.- Lingeman JE, Siegel YI, Steele B. Metabolic evaluation of infected renal lithiasis: clinical relevance. J Endourol. 1995; 9: 51-55.
45.- Ahlstrand C, Tiselius HG. Recurrences during a 10 years follow-up alter final renal stone episode. Urol Res. 1990; 18: 397-399.
46.- Avorn J, Winkelmayer WC, Bohn RL, Levin R, Glynn RJ, Levy E, Owen W. Delayed nephrologist referral and inadequate vascular access in patients with advanced kidney failure. J Clin Epi. 2002; 55: 711–716.
47.- Cimochowski GE, Worley E, Rutherford WE, Sartain J, Blondin J, Harter H. Superiority of the internal jugular over the subclavian access for temporary dialysis. Nephron. 1990; 54:154–161.
48.- National Kidney Foundation. K/DOQI clinical practice guidelines for vascular access, 2000. Am J Kidney Dis 2001; 37(suppl 1):S137-S181.
49.- Krzywda EA, Andris DA. Twenty-five Years of Advances in Vascular Access: Bridging Research to Clinical Practice Nutr Clin Pract. 2005; 20: 597-606.
50.- Mickley V. Central venous catheters: many questions, few answers. Nephrol Dial Transplant. 2000;17:1368–1373.
51.- MacRae JM, Ahmed A, Johnson N, Levin A, Kiaii M: Central vein stenosis: a common problem in patients on hemodialysis. ASAIO J. 2005;51:77–81.
52.- Stack AG. Impact of timing of nephrology referral and pre-ESRD care on mortality risk among new ESRD patients in the United States. Am J Kidney Dis. 2003; 41: 310–318.
53.- Roubicek C, Brunet P, Huiart L, Thirion X, Leonetti F, Dussol B, Jaber K, Andrieu D, Ramananarivo P, Berland Y. Timing of nephrology referral: Influence on mortality and morbidity. Am J Kidney Dis 2000;36: 35–41.
54.- Schwenger V, Morath C, Hofmann A, Hoffmann O, Zeier M, Ritz E. Late referral - a major cause of poor outcome in the very elderly dialysis patient. Nephrol Dial Transplant. 2006; 21: 962–967.
55.- Caskey FJ, Wordsworth S. Early referral and planned initiation of dialysis: what impact on quality of life? Nephrol Dial Transplant. 2003;18: 1330-1338.
56.- Traynor JP, Simpson K, Geddes CC, Deighan CJ, Fox JG. Early initiation of dialysis fails to prolong survival in patients with end-stage renal failure. J Am Soc Nephrol. 2002; 13:2125–2132.
57.- Fabrizi F, Lunghi G, Raffaele L, et al. Serologic survey for control of hepatitis C in haemodialysis patients: third-generation assays and analysis of costs. Nephrol Dial Transplant 1997;12:298-303.
58.- Flamm SL. Chronic hepatitis C virus infection. JAMA 2003;289:2413-2417.
59.- Petrosillo N, Gilli P, Serraino D, et al. Prevalence of infected patients and understaffing have a role in hepatitis C virus transmission in dialysis. Am J Kidney Dis 2001;37:1004-1010.
60.- Okuda K, Hayashi H, Kobayashi S, Irie Y. Mode of hepatitis C infection not associated with blood transfusion among chronic hemodialysis patients. J Hepatol. 1995;23:28-31.
61.- Huraib SO. Hepatitis C in dialysis patients. Saudi J Kidney Dis Transplant 2003; 14:442-50.
61- Tokars JI, Alter MJ, Arduino MJ. Nosocomial infections in hemodialysis units: strategies for control. In: Owen WF, Pereira BJG, Sayegh MH, eds. Dialysis and transplantation: a companion to Brenner and Rector's THE KIDNEY. Philadelphia, PA: W.B. Saunders Company, 2000:337—357
62-. Orth SR, Ogata H, Ritz E. Smoking and the kidney. Nephrol Dial Transplant. 2000; 15:1509–1511
63.- Orth SR: Smoking: A renal risk factor. Nephron 2000;86: 12–26.
64.- Halimi JM, Giraudeau B, Vol S, Caces E, Nivet H, Lebranchu Y, Tichet J. Effects of current smoking and smoking discontinuation on renal function and proteinuria in the general population. Kidney Int. 2000; 58: 1285–1292.
65.- Orth SR. Effects of Smoking on Systemic and Intrarenal Hemodynamics: Influence on Renal Function J Am Soc Nephrol 2004;15:S58-S63.
66.- Bleyer AJ, Shemanski LR, Burke GL, Hansen KJ, Appel RG. Tobacco, hypertension, and vascular disease: Risk factors for renal functional decline in an older population. Kidney Int. 2000;57: 2072–2079.
67.- Mohamed AO. Morbidity and mortality in ESRD patients on regular hemodialysis: a single center experience. Saudi J Kidney Dis Transpl. 2005;16:336-341
68.- Inrig JK, Sun JL, Yang Q, Briley LP, Szczech LA. Mortality by dialysis modality among patients who have end-stage renal disease and are awaiting renal transplantation. Clin J Am Soc Nephrol. 2006;1:774-779.
69.- Bradbury BD, Fissell RB, Albert JM, Anthony MS, Critchlow CW, Pisoni RL, Port FK, Gillespie BW. Predictors of early mortality among incident US hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Clin J Am Soc Nephrol. 2007;2:89-99.
70.- Waqar H. Kazmi, Gregorio T. Obrador, Samina S. KhanLate nephrology referral and mortality among patients with end-stage renal disease: a propensity score analysis Nephrol Dial Transplant. 2004; 19: 1808-1814
71.- Kovesdy CP. Regional mortality differences in end-stage renal disease: How far can observational studies take us? Kidney Int. (2007) 71, 11–12
Corresponding author: Dr. José Luis Rodríguez López
jluisr5106 @ yahoo.es.
Received: December 14, 2007. Received reviewed: April 8, 2008
Published June 12, 2008
