Indice del volumen
Volume index
Comité Editorial
Editorial Board
Comité Científico
Scientific Committee
Rev Electron Biomed / Electron J Biomed 2013;1:50-55.
Letter:
ON AGE DEPENDENCE OF PERIPHERAL
AUGMENTATION INDEX.
Jose Luis Hernandez Caceres PhD.
Department of Basic Biomedical Sciences,
School of Medicine and Allied Health Sciences.
University of The Gambia
Banjul. The Gambia
cacerjlh @ yahoo.com
Sir:
The possibility to continuously assess changes in blood pressure dictates the need to find proper ways of obtaining clinically relevant information from such signals. In the simplest linear case scenario pressure changes are directly proportional to volume changes. This could give some theoretical soundness to the use of photoplethysmographic signals for similar purposes1. Even when the PPG signal is not a "purely volumetric" signal, the fact that it is at least partially related to volume, can justify , in the sense of the Takens theorem, its use as a surrogate of continuous pressure signal. If this will work in practice, the amount of resources saved and the number of patients potentially evaluated can increase substantially.
Augmentation Index (AIx) has been widely used as a purported indicator of arterial stiffness. AIx is defined as the proportion of the second, reflected wave to the systolic wave. In particular it has been shown that peripheral AI (pAIx) reliably reflects the relationship between central and peripheral pulse pressure2. Plausibly, AIx seems to measure the contribution of an early and substantial reflected wave superposed to an incident wave. It seems also reasonable to expect that the AIx will increase with both higher amplitude of the reflected wave as well as with a higher pulse wave velocity.
On the other hand, it is known that both the amplitude and velocity of the reflected wave tend to increase with age and this would lead to steady increases in AIx with age3. Indeed, a positive age correlation has been confirmed in some reports4. Unexpectedly, there are various reports claiming that AI is not always significantly correlated with age. Some attempts to explain this fact have been put forward based on both mathematical5 and physiological grounds6.
Here, age dependence of pAIx assessed from Photoplethysmographic signals recorded from a sample of purportedly healthy subjects (10-87 y) is addressed. Also, a simulation study was carried out to clarify the possible relationship between peripheral pAIx and both amplitude- and velocity of the reflected wave.
Subjects. Fifty three volunteers were recruited in the city of Orense. They were free of clinical cardiovascular disease and medication, and Body Mass Index never surpassed 31 kgxm-2. Approval was obtained from the local research ethics committee, and written informed consent was obtained from all participants. Five-min-duration photoplethysmographic signals were obtained from the pointer finger of the right arm with the subject in supine position, using a validated oximeter (Nellcor 395, USA). Signals were digitized at 100 Hz and saved as ASCII files. Continuous pulse pressure signals digitized at 125 were downloaded from the "Fantasia" data base available at www.physionet.org.
Data analysis. Peripheral AIx determination. AI was estimated over an average wave obtained automatically from the superposition of at least 65 individual waves. For wave averaging, a pattern vector of length L (usually about 90 data points) was picked by visual inspection. Correlations were measured between the pattern vector and each individual vector of length L starting at the point I of the original signal. The obtained vector of correlations (corresponding to about 100 seconds of recording) was then submitted to further analysis. Those vectors with from the signal having a correlation higher than a certain threshold "Th" and corresponding to a local maximum of correlation were picked as individual waves and entered as rows of the matrix M of the waveforms. From M the average waveform was obtained from averaging over all rows. The main virtue of the method is that a representative wave is obtained without the need to rely on subjective opinions of experts. After estimating the first and second derivatives of the average wave, the inflexion points were determined. Peripheral AIx was obtained as the ratio of the amplitude at the inflexion point to the right of the peak to the maximum amplitude2.
Simulations. The systolic part of the PPG wave was represented as the composition of an incident and a reflected wave. Expecting minor loss of generalization, each individual wave was simulated with a bell shaped symmetrical and infinitely derivable curve of the type:
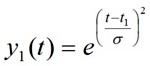
The relative amplitude of the reflected wave (a) changed from zero to 1; the value of t1 was fixed in our simulations at 40 (corresponding to 400 ms). For t2, values ranged between 46 and 65 (roughly corresponding to velocities between 4 and 17 m/s for a sampling rate of 100 Hz and a distance of 1 m between abdominal aortic bifurcation and the pointer finger). Aix was determined from these simulated signals using the same algorithm as the one used for average waves.
Statistical analysis. Linear and nonlinear regression was indicated in some scatter plots, whereas other data are presented as means and standard deviations.
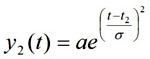
Correlation of p AIX with age. Our data exhibited a negative correlation between pAIx and age (r=-0.505; p=0.0039; Figure 1). Since the PPG signal is a mere surrogate of pulse pressure, this result can be a consequence of the poor quality of the PPG signal as a proxy for pulse pressure signals.
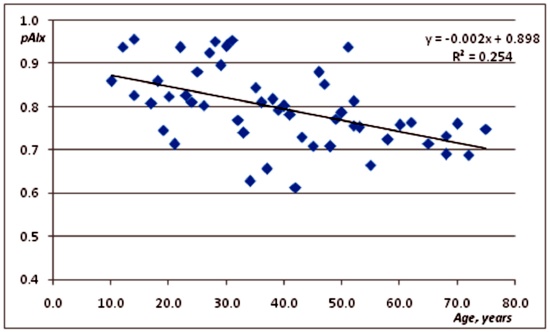
Figure 1. Scatter plot relating peripheral augmentation index as a function of age.
Thus we decided to explore if pAIx changes with age in a sample of clinically healthy young and elderly patients recorded with a continuous pulse pressure technique. Data were downloaded from the "Fantasia" database at physionet.org.
Results did not support the hypothesis of higher pAIx values among elderly patients. Here pAIx was estimated at 0.80 ± 0.16 among young subjects and 0.82 ± 0.11 among elderly (n. s. nonparametric permutation test)
After confirming that pAIx does not necessarily increases as age increases, the next step was to explore if a model wave composed of an incident and a superposed reflected wave will behave as intuitively expected.
For a comprehensive answer to this question, different waveforms shapes and a large set of possible parameters configurations need to be explored. In this case we explored the simple case of two symmetrical and infinitely derivable waves represented by a Gaussian-like function. (See methods section). We tried to make the wave duration comparable to that in real recordings (about 100 data points corresponding to 1000 ms with a 100 Hz sampling rate).
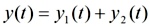
Fixing the velocity at 5 m/s (corresponding to a 200 ms time shift for a standard distance of 1 meter between aorta bifurcation and pointer finger) and changing the reflected wave amplitude, it was obtained that the simulated AIx steadily increases with amplitude (figure..) In this case the results from numerical experiments are coincident with the apparent expectations. Similar results are obtained if velocity is fixed at 20 m/s.
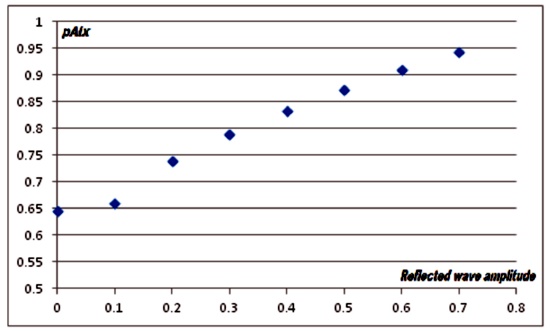
Figure 2 Simmulation results for the dependence of peripheral augmentation index respect to amplitude of the refected wave.
Amplitude of the incident wave was set =1.
When fixing the amplitude of the reflected wave at 0.3 times the amplitude of the incident wave, a nonlinear dependence of AIx respect to wave velocity is obtained for the velocity range from 4 to 17 m/s (figure 3).
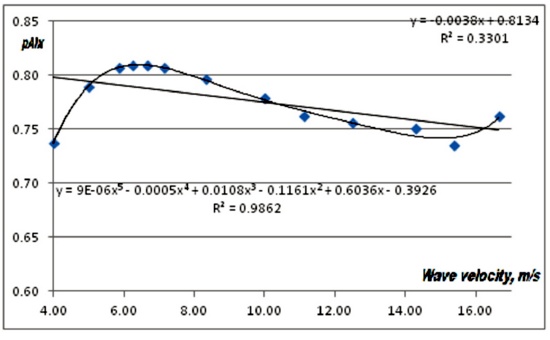
Figure 3. Simmulation results for the dependence of peripheral augmentation index respect to wave velocity.
Linear fit shos a tendency to reduction as velocity increases, whereas a 5th degree polynomial fit suggest a nonmonotonous dependence.
As apparent from figure 3, depending on the velocity range AIxcan either increase (e. g. from 4 to 6 m/s or from 15 to 17 m/s)) or decrease (from 7 to14 m/s) of remain almost unchanged (from 5 to 7 m/s). The general trend for the whole range of velocities is decreasing. Even when these numerical experiments cannot be taken at "face value" they can provide a good explanation for the observed decrease of AIx with age.
Thus far, this is the first report of a negative correlation between pAIx and age. The used data sample is characterized by a very homogenous ethnic and cultural origin (mostly citizens from Orense, a city at the heart of Galicia having a low rate of inmigrantion. Ethnic differences have been documented for AIx developmental equations7. However, this cannot be the only factor for the obtained results. At any rate, a brief review of literature can suggest that the claim about a positive correlation between AIx and age does not enjoy a great support. Thus some authors claim that the correlation is strongest for ages below 50 years, vanishing for older ages8-9. Moreover, some authors have hypotesized a decreasing wave reflection in older persons10. On the other hand, some authors have found a negligible role of AIx as a surrogate for arterial stiffness under adrenergic estimulation11. In other studies, multivariate analysis has found no correlation with age for AIx12.
Working with rabbits, it was found a non-significant correlation between Aix and age. Moreover, as arteriosclerosis progressed and arteries stiffened, this did not affect the AIx13. Similar results were obtained in humans14-15.
In another report4 it was found that age significantly correlated with augmentation index only in healthy subjects but not in those with atherosclerotic disease. Additionally those authors found that augmentation index is not correlated with the presence of vasoactive medication in subjects without atherosclerotic disease.
It is not excluded that the inverse relation reported between AIx and height is an indirect consequence of an increase in AIx after an increase in time shift for the reflected wave, as documented from our simulations.
Such diversity of results can put in doubt the validity of this index as a marker of cardiovascular function. Results of our simulations can at least partially explain this diversity of results. As shown in figure 3 depending on the range of pulse waves to be regarded, the relationship between AI and arterial stiffness can be either positive, negative or nil.
The European Society of Cardiology-European Society of Hypertension guidelines of the year 2007 attribute to consequences of arterial stiffness and wave reflection a major role on cardiovascular mortality16. But the authors claimed the "poor availability of devices and methods providing easy and widely suitable measuring of arterial wall stiffness or their surrogates like augmentation index (AIx)". However, our results are not supportive of AIx being a good candidate for such a role. Particularly, it seems that the validity of AIx as a vascular index needs more substantial support; it is not excluded that other new indices are required for assessing vascular function and its decline with age and pathological condition.
REFERENCES
1. Korpas D, Hálek J, Doleal L. Parameters Describing the Pulse Wave. Physiol Res. 2009; 58: 473-479.
2. Shahzad M, Guilcher A, Kamalesh T, Clapp B, Redwood S, Marber M, Chowienczyk P. Peripheral Augmentation Index Defines the Relationship Between Central and Peripheral Pulse p ressure. Hypertension. 2008; 51:112-118.
3. Weber T, Auer J, O'Rourke MF, Kvas E, Lassnig E, Berent R. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation. 2004;109: 184-189.
4. Nürnberger J; Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schäfers RF. Augmentation index is associated with cardiovascular risk. Journal of Hypertension. 2002; 20(12 ):2407-2414.
5. Namasivayam M, Adji A, O'Rourke MF. Aortic Augmentation Index and Aging: Mathematical Resolution of a PhysiologicalDilemma? Hypertension. 2010;56:e9-e10.
6. . McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockroft JR.Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial. J Am Coll Cardiol. 2005; 46:1753-1760.
7. Chirinos JA, Kips JG, Roman MJ, Medina-Lezama J, Li Y, Woodiwiss AJ, Norton GR, Yasmin, Van Bortel L, Wang JG, Cockcroft JR, Devereux RB, Wilkinson IB, Segers P, McEniery CM. Ethnic Differences in Arterial Wave Reflections and Normative Equations for Augmentation Index. Hypertension. 2011;57:1108-1116.
8. Wojciechowska W, Staessen JA, Nawrot T, Cwynar M, Seidlerova J, Stolarz K, Gasowski J, Ticha M, Richart T, Thijs L, Grodzicki T, Kawecka-Jaszcz K, Filipovsky J. Reference values in white Europeans for the arterial pulse wave recorded by means of the SphygmoCor device. Hypertens Res. 2006;29:475- 483.
9. Fantin F, Mattocks A, Bulpitt CJ, Banya W, Rajkumar C. Is augmentationindex a good measure of vascular stiffness in the elderly? Age Ageing. 2007; 36:43- 48.
10. Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA,Vasan RS, Levy D. Changes in arterial stiffness and wave reflection withadvancing age in healthy men and women: the Framingham Heart Study. Hypertension. 2004; 43:1239 -1245.
11. Lemogoum D, Flores G, Van den Abeel W, Ciark A, Leeman M, Degaute JP, van de Born P, Van Bortel L. Validity of pulse pressure and augmentation index as surrogate measures of arterial stiffness during beta-adrenergic stimulation. Journal of Hypertension. 2004, 22(3): 511-517.
12. Nürnberger J, Dammer S, Opazo Saez A, Philipp T, Schäfers RF. Diastolic blood pressure is an important determinant of augmentation index and pulse wave velocity in young, healthy males. Journal of Human Hypertension. 2003; 17:153-158.
13. Katsuda SI, Miyake M, Kobayashi D, Hazama A, Kusanagi M, Takazawa K. Does the Augmentation Index of Pulse Waves Truly Increase With Progression of Atherosclerosis? An Experimental Study With Hypercholesterolemic Rabbits. Am J Hypertens. 2013; 26 (3): 311-317
14. Hope SA, Antonis P, Adam D, Cameron JD, Meredith I: Arterial pulse wave velocity but not augmentation index is associated with coronary artery disease extent and severity: implications for arterial transfer function applicability. J Hypertens. 2007; 25: 2105-2109.
15. Lacy PS, O'Brien DG, Stanley AG, Dewar MM, Swales PPR, Williams B. Increased pulse wave velocity is not associated with elevated augmentation index in patients with diabetes. Journal of Hypertension. 2004; 22(10): 1937-1944.
16. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G et al. Guidelines for the management of arterial hypertension. Eur Heart J. 2007; 28: 1462-1536
CORRESPONDENCE:
Jose Luis Hernandez Caceres
Department of Basic Biomedical Sciences,
School of Medicine and Allied Health Sciences
University of The Gambia
Banjul.
The Gambia
Mail:cacerjlh @ yahoo.com
