Indice del volumen Volume index
Comité Editorial Editorial Board
Comité Científico Scientific Committee
- Extrinsic or by external compression of the urinary tract
- tumors / retroperitoneal adenomegaly (ureteral compromise)
- retroperitoneal fibrosis (compromiso ureteral): aneurism of the abdominal aorta, Crohn's disease.
- prostatic neoplasia: hyperplasia (compression of the prostatic urethra), carcinoma (ureteral compromiso due to infiltration of the trígono vesical)
- gynecological pathology: neoplasia, prolapse, endometrosis
- inadvertent surgical ureteral binding
- oIntrinsic or inherent to the urinary tract:
- a. Intraluminal: urinary calculus (pelvis and/or ureter), clots, papillary necrosis, fungal ball.
- b. Intra-mural: condition of the ureteral soft muscle, it can be
- functional: illness (diabetes mellitus, parkinsons, spinal medullary lesion, etc.), drugs (anticholinergic, levo-dopa)
- structural: tuberculosis, ureteral narrowness/urethral, neoplasia
OBSTRUCTIVE NEPHROPATHY:
ITS PHYSIOPATHOLOGY
Carlos G. Musso1,2, Matilde Navarro1, Ricardo Jauregui1,2
1Renal Physiology Section. Nephrology Division.
Hospital Italiano de Buenos Aires.
2Hospital Italiano de San Justo Agustín Rocca
Buenos Aires. Argentina
carlos.musso @ hospitalitaliano.org.ar
Rev Electron Biomed / Electron J Biomed 2011;2: 57-61.
Comment of the reviewer Abdias Hurtado Arestegui MD. . Servicio de Nefrología Hospital Nacional Arzobispo Loayza. Universidad Peruana Cayetano Heredia. Lima. Peru
Comment of the reviewer Jesus Garrido MD. Responsável pelo Sector de Hemodiálise. Unidade de Nefrologia e Diálise, Hospital de São Teotónio, Viseu - Portugal. Director Clínico. Diaverum-Unidade da Régua. Peso da Régua. Portugal.
SUMMARY:
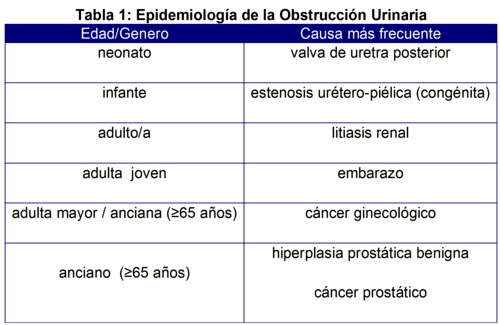
Obstructive nephropathy is the functional and /or parenchymal renal damage secondary to the urinary tract occlusion at any part of it. The inducing urinary obstruction diseases can vary depending on the patient´s age and gender.
There are many renal dysfunction inducing mechanisms involved in this entity: increase in the intra-luminal pressure, ureteral dilatation with ineffective ureteral peristalsis, glomerular ultrafiltration net pressure reduction, intra-renal glomerular blood flux reduction due to vasoconstriction, and local disease of chemotactic substances. Obstructive nephropathy can also lead to hypertension (vasoconstriction-hypervolemia), hyperkalemia, metabolic acidosis (aldosterone resistance), diabetes insipidus (vasopressine resistance).
In conclusion, since obstructive nephropathy is a potentially reversible cause of renal dysfunction, it should always be taken into account among the differential diagnosis of renal failure inducing mechanisms.
KEYWORDS: Obstructive nephropathy. Renal dysfunction. Physiopathology.
RESUMEN:
Por nefropatía obstructiva se entiende el daño funcional y/o parenquimatoso renal secundario a la obstrucción del tracto urinario en cualquier sector de su longitud. Las entidades que conducen a la misma varían según la edad y el género del paciente.
Fisiopatológicamente, son varios los mecanismos que llevan al compromiso de la función renal en este disturbio: aumento de la presión intraluminal, dilatación ureteral y en consecuencia peristalsis ureteral inefectiva y oposición a la presión neta de ultrafiltración glomerular, vasoconstricción intrarenal con la consiguiente reducción en el flujo sanguíneo glomerular, liberación de sustancias quimiotácticas que atraen monocitos y macrófogos que liberan localmente proteasas y radicales libres. Durante una uro-obstrucción puede además desencadenarse hipertensión arterial (vasocontricción-hipervolemia), hiperkalemia, acidosis metabólica (resistencia a la aldosterona) y diabetes insípida (resistencia a la vasopresina).
Concluimos que la uropatía obstructiva es un mecanismo de insuficiencia renal, que dada su relativa simplicidad para ser resuelto, debe ser siempre tenido en cuenta entre los diagnósticos diferenciales del fracaso renal.
PALABRAS CLAVE: Nefropatía obstructiva. Insuficiencia renal. Fisiopatología.
Introduction:
Obstructive nephropathy is the functional and/or renal parenchymatous damage secondary to the obstruction of the urinary tract in any sector along its length and which can be the potential cause of acute as well as chronic renal failure. In the same way, when such obstruction is located in any point between the renal pelvis and the distal end of the urethra, it receives the more specific name of obstructive uropathy. It is worth mentioning that hydronephrosis is the expansion of the pelvis and renal calyces proximal to the obstruction point; and that expansion is not always synonym of obstruction, since there are non-obstructive types of expansion known as ectasias1 (Tabla 1)
Physiopatology2-4:
The obstruction of the urinary flow can take place inside the renal tubules as well as in any other segment of the urinary tract (renal pelvis, ureter, bladder and urethra). Independently of the place where the urinary obstruction happens, and from this moment, a series of events start to happen, which if they are not corrected can lead, in time, to irreversible renal damage and tubular atrophy. After an obstruction has settled, there is an increase in the pressure corresponding to its proximal section, due to the effect of the net glomerular filtration pressure, which leads to an increase in intraluminal pressure, that carries a progressive expansion of the ureter as a compensating mechanism (ley de la Lapace), thus the significant difference of pressure between the ureter in a state of contraction and at rest is reduced, resulting in an ineffective ureteral peristalsis. Sometimes there is a rapture of the renal calices with the subsequent formation of urinomas.
On the other hand, such pressure is transmitted to the tubular sectors proximal to the obstruction causing a reduction of the glomerular filtration since it counteracts to the glomerular filtration net pressure. In this sense, it should be taken into consideration that the glomerular filtration is the result of a game of pressures which are established in the glomerular capillaries and the Bowman capsule, where in favor of the filtration we find the hydrostatic pressure of the capillary (very important) and the oncotic pressure of the Bowman capsule (minimum), while against it we find the oncotic pressure of the capillary (considerable) and the hydrostatic pressure of the Bowman capsule (minimum). Usually glomerular hydrostatic pressure is largely predominant, on whom the net ultrafiltration pressure depends almost completely. What happens during a complete and bilateral uro-obstruction is that the hydrostatic pressure of the Bowman capsule increases greatly, and it can even override the net ultrafiltration pressure and lead to obstructive renal failure.
On the other hand, the above mentioned increase in intratubular pressure initially induces the release of vasodilating prostaglandins which dilate the afferent arteriole thus incrementing the renal flow by 40%. Nevertheless, if the obstruction is sustained in time, it leads to intrarenal vasoconstriction with the subsequent reduction in the glomerular blood flow. This phenomenon could be mediated by the release of angiotensin II and tromboxane by the obstructed nephrons. The consequence of this last phenomenon is that it avoids the perfusion of the non-functioning nephrones by means of the redistribution of flow towards those who are functioning.
In the case of severe and prolonged urinary obstructions, the renal parenchyma is reduced to a thin ring of atrophic tissue mainly as a consequence of the ischemia suffered by its continuous hyperfusion. It is also stated that the damaged tubules release a chemotactic substance which would attract monocytes and macrophagues, which would infiltrate the renal parenchyma, damaging it by means of the local release of proteases and free radicals.
An uro-obstruction can also cause hypertension which at its first stage in general is mediated by the activation of the renine-angiotensin-aldosterone system (vasoconstriction) and later, if a total obstruction occurs it is mainly due to water and salt retention (hypervolemia). Likewise, the urinary obstruction can lead to a dysfunction of the distal nephron sectors (resistance to aldosterone and vasopresin), making it difficult for the local secretion of potassium and protons, as well as reducing the water reabsorption, thus facilitating the development of hyperkalemia, hyperchloremic metabolic acidosis and nephrogenic diabetes insipidus, respectively. The latter causes polyuria which is characteristic of partial obstructive uropathy. In the case of intratubular obstructions (uric acid, pigments, etc.), to the physiopathological phenomena described above it is necessary to add the fact that these toxic substances also generate local tubular damage of the toxic-ischemic type by favouring the local formation of free radicals and vasoconstriction.
Regarding the urinary obstruction mechanisms, it is possible to divide them into those which are intra-renal (intratubular) and those which are extra-renal. The latter can be subdivided into those which have intrinsic and extrinsic causes to the urinary tract 5-6:
Urinary desobstruction: fisiopathology and consequences 7:
Data obtained from tests performed in animal models and information obtained from the evolution of clinical cases, suggest that the resolution of a complete obstruction before 8 -14 weeks after it has settled can achieve a total recovery of the glomerular filtration. A later resolution can mean partial or nule recovery, depending on the evolution time of the obstruction, the age of the patient and the degree of damage to the renal function previous to the obstruction.
After the resolution of a bilateral obstruction or a unilateral one in a patient with only one kidney, it is normal to find elevated serum levels of atrial factors, tubular resistance to vasopressin (reduction of the expression of aquaporin 2 channels in the collecting tubules and compromise of the medullar tonicity), decrease in the tubular reabsorption capacity of sodium and urea and presence of a free urinary tract, so the osmotic diuretic effect of the not reabsorbed urea and sodium starts to act, which increment diuresis finally leading to potassium, calcium, magnesium and phosphorus expoliation, which puts the patient at risk of having severe hydroelectrolytic depletion if these losses are not adequately monitored and treated. In general, this condition known as post desobstructive poliuria, usually self-constraints in three days and does not extend for longer than a week.
Conclusion:
Obstructive uropathy is a mechanism of renal insufficiency, which since it is relatively simple to solve, should always be taken into consideration as one of the differential diagnosis of renal failure.
REFERENCES
-
1.- Clarkson M, Magee C, Brenner B. Obstructive nephropathy. In Clarkson M, Magee C, Brenner B (Eds.). Brenner & Rector. The Kidney. Philadelphia. Saunders. 2010: 332-344
2.- Rennke H, Denker B. Tubulointerstitial diseases. In Rennke H, Denker B (Eds.) Renal pathophysiology. The essentials. Philadelphia. Lippincott Williams & Wilkins. 2007: 337-360
3.- Alivizatos G, Skolarikos A. Obstructive uropathy and benign prostatic hyperplasia. In Macías Núñez J, Cameron S, Oreopoulos D (Eds.) The aging kidney in health and disease. New York. Springer. 2008: 257-272
4.- Sorensen M, Stoller M. Obstructive uropathy. En Lerma E, Nissenson A (Eds.). Nephrology secrets. Elsevier Mosby. 2012: 119-122
5.- Vela Navarrete R. El riñón dilatado. Barcelona. Masson. 2001
6.- Klahr S. Urinary tract obstruction. In Schrier R (Ed.). Disease of the kidney & urinary tract. Philadelphia. Kluwer. Lippincott Williams & Wilkins. 2007: 689-716
7.- Vela Navarrete R. Uropatía obstructiva. En Hernando Avendaño L. (Eds.) Nefrología clínica. Buenos Aires. Panamericana. 2009: 544-564
CORRESPONDENCE:
Carlos G. Musso
Sección Fisiología Clínica Renal. Servicio de Nefrología y Medio Interno.
Hospital Italiano de Buenos Aires.
Buenos Aires. Argentina
Email: carlos.musso @ hospitalitaliano.org.ar

 1 (TGF
1 (TGF